Emens, L. A. et al. Challenges and opportunities in cancer immunotherapy: a Society for Immunotherapy of Cancer (SITC) strategic vision. J. Immunother. Cancer 12, e009063 (2024).
Atkins, M., Kunkel, L., Sznol, M. & Rosenberg, S. High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: long-term survival update. Cancer J. Sci. Am. 6, 11–14 (2000).
Yang, J. C. et al. Randomized study of high-dose and low-dose interleukin-2 in patients with metastatic renal cancer. J. Clin. Oncol. 21, 3127–3132 (2003).
He, X. & Xu, C. Immune checkpoint signaling and cancer immunotherapy. Cell Res. 30, 660–669 (2020).
Irvine, D. J., Maus, M. V., Mooney, D. J. & Wong, W. W. The future of engineered immune cell therapies. Science 378, 853–858 (2022).
Rosenberg, S. A. & Restifo, N. P. Adoptive cell transfer as personalized immunotherapy for human cancer. Science 348, 62–68 (2015).
Awasthi, R., Maier, H. J., Zhang, J. & Lim, S. Kymriah® (tisagenlecleucel)–An overview of the clinical development journey of the first approved CAR-T therapy. Hum. Vaccin. Immunother. 19, 2210046 (2023).
Julve, M., Lythgoe, M. P., Larkin, J. & Furness, A. J. S. Lifileucel: the first cellular therapy approved for solid tumours. Trends Cancer 10, 475–477 (2024).
Monberg, T. J., Borch, T. H., Svane, I. M. & Donia, M. TIL therapy: facts and hopes. Clin. Cancer Res. 29, 3275–3283 (2023).
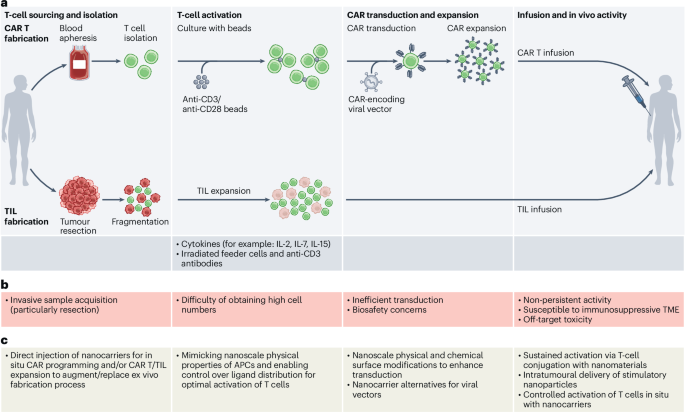
Liu, Y., Sperling, A. S., Smith, E. L. & Mooney, D. J. Optimizing the manufacturing and antitumour response of CAR T therapy. Nat. Rev. Bioeng. 1, 271–285 (2023).
Matsueda, S., Chen, L., Li, H., Yao, H. & Yu, F. Recent clinical researches and technological development in TIL therapy. Cancer Immunol. Immunother. 73, 232 (2024).
Hyun, J., Kim, S. J., Cho, S. D. & Kim, H. W. Mechano-modulation of T cells for cancer immunotherapy. Biomaterials 297, 122101 (2023).
Wang, F. Y., Qiu, T., Ling, Y., Yang, Y. & Zhou, Y. Physical and chemical cues at the nano–bio interface for immunomodulation. Angew. Chem. 61, e202209499 (2022).
Eshhar, Z., Waks, T., Gross, G. & Schindler, D. G. Specific activation and targeting of cytotoxic lymphocytes through chimeric single chains consisting of antibody-binding domains and the gamma or zeta subunits of the immunoglobulin and T-cell receptors. Proc. Natl Acad. Sci. USA 90, 720–724 (1993).
Kalos, M. et al. T cells with chimeric antigen receptors have potent antitumor effects and can establish memory in patients with advanced leukemia. Sci. Transl. Med. 3, 95ra73 (2011).
FDA approves obecabtagene autoleucel for adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia. US Food and Drug Administration https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-obecabtagene-autoleucel-adults-relapsed-or-refractory-b-cell-precursor-acute (2024).
Juan, M., Delgado, J., Calvo, G., Trias, E. & Urbano-Ispizua, Á. Is hospital exemption an alternative or a bridge to european medicines agency for developing academic chimeric antigen receptor T-cell in Europe? Our experience with ARI-0001. Hum. Gene Ther. 32, 1004–1007 (2021).
Damodar, S. et al. Early results from a phase-2 study of varnimcabtagene autoleucel (IMN-003A), a first-in-India industry CD19-directed CAR-T cell therapy with fractionated infusions for patients with relapsed and/or refractory B cell malignancies (IMAGINE study). Blood 140, 10343–10344 (2022).
Oliver-Caldes, A. et al. Biomarkers of efficacy and safety of the academic BCMA-CART ARI0002h for the treatment of refractory multiple myeloma. Clin. Cancer Res. 30, 2085–2096 (2024).
Nie, T. Talicabtagene autoleucel: first approval. Mol. Diagn. Ther. 28, 495–499 (2024).
Therapeutics announces NMPA approval of the supplemental biological license application for Carteyva in adult patients with relapsed or refractory mantle cell lymphoma. JW Therapeutics https://www.jwtherapeutics.com/en/media/press-release/20240827/ (2024).
Wang, Y. et al. Inaticabtagene autoleucel in adult relapsed or refractory B-cell acute lymphoblastic leukemia. Blood Adv. 9, 836–843 (2025).
Saez-Ibañez, A. R. et al. The changing landscape of cancer cell therapies: clinical trials and real-world data. Nat. Rev. Drug Discov. 23, 736–737 (2024).
Rosenberg, S. A., Spiess, P. & Lafreniere, R. A new approach to the adoptive immunotherapy of cancer with tumor-infiltrating lymphocytes. Science 233, 1318–1321 (1986).
Diorio, C., Teachey, D. T. & Grupp, S. A. Allogeneic chimeric antigen receptor cell therapies for cancer: progress made and remaining roadblocks. Nat. Rev. Clin. Oncol. 22, 10–27 (2025).
Hopewell, E. L., Cox, C., Pilon-Thomas, S. & Kelley, L. L. Tumor infiltrating lymphocytes streamlining a complex manufacturing process. Cytotherapy 21, 307–314 (2018).
Flugel, C. L. et al. Overcoming on-target, off-tumour toxicity of CAR T cell therapy for solid tumours. Nat. Rev. Clin. Oncol. 20, 49–62 (2022).
Albelda, S. M. CAR T cell therapy for patients with solid tumours: key lessons to learn and unlearn. Nat. Rev. Clin. Oncol. 21, 47–66 (2023).
Zhao, Y. et al. Tumor infiltrating lymphocyte (TIL) therapy for solid tumor treatment: progressions and challenges. Cancers 14, 4160 (2022).
Madkour, L. H. in Nanoelectronic Materials: Fundamentals and Applications (ed. Madkour, L. H.) 1–47 (Springer, 2019).
Mitchell, M. J. et al. Engineering precision nanoparticles for drug delivery. Nat. Rev. Drug Discov. 20, 101–124 (2020).
Joyce, P. et al. A translational framework to DELIVER nanomedicines to the clinic. Nat. Nanotechnol. 19, 1597–1611 (2024).
Anselmo, A. C. & Mitragotri, S. Nanoparticles in the clinic: an update post COVID-19 vaccines. Bioeng. Transl. Med. 6, e10246 (2021).
Hou, F., Guo, Z., Ho, M. T., Hui, Y. & Zhao, C. X. Particle-based artificial antigen-presenting cell systems for T cell activation in adoptive T cell therapy. ACS Nano 18, 8571–8599 (2024).
Hu, T., Kumar, A. R. K., Luo, Y. & Tay, A. Automating CAR-T transfection with micro and nano-technologies. Small Methods 8, e2301300 (2024).
Sunshine, J. C. & Green, J. J. Nanoengineering approaches to the design of artificial antigen-presenting cells. Nanomedicine 8, 1173–1189 (2013).
Dahotre, S. N., Romanov, A. M., Su, F. Y. & Kwong, G. A. Synthetic antigen-presenting cells for adoptive T cell therapy. Adv. Ther. 4, 2100034 (2021).
Ben-Akiva, E. et al. Shape matters: biodegradable anisotropic nanoparticle artificial antigen presenting cells for cancer immunotherapy. Acta Biomater. 160, 187–197 (2023).
Perica, K. et al. Nanoscale artificial antigen presenting cells for T cell immunotherapy. Nanomedicine 10, 119–129 (2014).
Isser, A. et al. Nanoparticle-based modulation of CD4+ T cell effector and helper functions enhances adoptive immunotherapy. Nat. Commun. 13, 6086 (2022).
Ichikawa, J. et al. Rapid expansion of highly functional antigen-specific T cells from patients with melanoma by nanoscale artificial antigen-presenting cells. Clin. Cancer Res. 26, 3384–3396 (2020).
Lee, K. & Yu, Y. Janus nanoparticles for T cell activation: clustering ligands to enhance stimulation. J. Mater. Chem. B 5, 4410–4415 (2017).
Matic, J., Deeg, J., Scheffold, A., Goldstein, I. & Spatz, J. P. Fine tuning and efficient T cell activation with stimulatory aCD3 nanoarrays. Nano Lett. 13, 5090–5097 (2013).
Guasch, J., Muth, C. A., Diemer, J., Riahinezhad, H. & Spatz, J. P. Integrin-assisted T-cell activation on nanostructured hydrogels. Nano Lett. 17, 6110–6116 (2017). This work proposes that the nanoscale arrangement of anti-CD3 and integrin-binding ligands can be strategically engineered to modulate T cell activation.
Pinheiro, A. V., Han, D., Shih, W. M. & Yan, H. Challenges and opportunities for structural DNA nanotechnology. Nat. Nanotechnol. 6, 763–772 (2011).
Teixeira, A. I. et al. Spatial regulation of T-cell signaling by programmed death-ligand 1 on wireframe DNA origami flat sheets. ACS Nano 15, 3441–3452 (2021).
Hellmeier, J. et al. DNA origami demonstrate the unique stimulatory power of single pMHCs as T-cell antigens. Biophys. J. 120, 330a (2021).
Cheung, A. S., Zhang, D. K. Y., Koshy, S. T. & Mooney, D. J. Scaffolds that mimic antigen-presenting cells enable ex vivo expansion of primary T cells. Nat. Biotechnol. 36, 160–169 (2018).
Fadel, T. R. et al. A carbon nanotube-polymer composite for T-cell therapy. Nat. Nanotechnol. 9, 639–647 (2014).
Jie, J., Mao, D., Cao, J., Feng, P. & Yang, P. Customized multifunctional peptide hydrogel scaffolds for CAR-T-cell rapid proliferation and solid tumor immunotherapy. ACS Appl. Mater. Interfaces 14, 37514–37527 (2022).
Lambert, L. H. et al. Improving T cell expansion with a soft touch. Nano Lett. 17, 821–826 (2017).
Mandal, S. et al. Polymer-based synthetic dendritic cells for tailoring robust and multifunctional T cell responses. ACS Chem. Biol. 10, 485–492 (2015).
Aramesh, M. et al. Nanoconfinement of microvilli alters gene expression and boosts T cell activation. Proc. Natl Acad. Sci. USA 118, e2107535118 (2021).
Bhingardive, V. et al. Antibody-functionalized nanowires: a tuner for the activation of T cells. Nano Lett. 21, 4241–4248 (2021).
Esmaeili, F. et al. Spiky gold nanoparticles, a nanoscale approach to enhanced ex vivo T-cell activation. ACS Nano 18, 21554–21564 (2024).
Lei, K., Kurum, A. & Tang, L. Mechanical immunoengineering of T cells for therapeutic applications. Acc. Chem. Res. 53, 2777–2790 (2020).
Perica, K. et al. Magnetic field-induced T cell receptor clustering by nanoparticles enhances T cell activation and stimulates antitumor activity. ACS Nano 8, 2252–2260 (2014).
Liu, Z. et al. Nanoscale optomechanical actuators for controlling mechanotransduction in living cells. Nat. Methods 13, 143–146 (2016).
Zheng, Y. et al. Optoregulated force application to cellular receptors using molecular motors. Nat. Commun. 12, 3580 (2021).
Fu, D. et al. Mechanically optimize T cells activation by spiky nanomotors. Front. Bioeng. Biotechnol. 10, 844091 (2022).
Chada, N. C. & Wilson, J. T. Jump-starting chimeric antigen receptor-T cells to go the extra mile with nanotechnology. Curr. Opin. Biotechnol. 89, 103179 (2024).
Belling, J. N. et al. Acoustofluidic sonoporation for gene delivery to human hematopoietic stem and progenitor cells. Proc. Natl Acad. Sci. USA 117, 10976–10982 (2020).
Sytsma, B. J. et al. Scalable intracellular delivery via microfluidic vortex shedding enhances the function of chimeric antigen receptor T-cells. Sci. Rep. 15, 5749 (2025).
Aramesh, M. et al. Enhanced cellular uptake through nanotopography-induced macropinocytosis. Adv. Funct. Mater. 34, 2400487 (2024).
Pan, H. et al. Glycometabolic bioorthogonal chemistry-guided viral transduction for robust human T cell engineering. Adv. Funct. Mater. 29, 1807528 (2019).
Chen, Y. et al. Efficient non-viral CAR-T cell generation via silicon-nanotube-mediated transfection. Mater. Today 63, 8–17 (2023).
Shokouhi, A. R. et al. Engineering efficient CAR-T cells via electroactive nanoinjection. Adv. Mat. 35, e2304122 (2023).
Tay, A. & Melosh, N. Mechanical stimulation after centrifuge-free nano-electroporative transfection is efficient and maintains long-term T cell functionalities. Small 17, 2103198 (2021).
Xiong, R. et al. Fast spatial-selective delivery into live cells. J. Control. Release 266, 198–204 (2017).
Pinto, I. S., Cordeiro, R. A. & Faneca, H. Polymer- and lipid-based gene delivery technology for CAR T cell therapy. J. Control. Release 353, 196–215 (2023).
Selby, L. I., Cortez-Jugo, C. M., Such, G. K. & Johnston, A. P. R. Nanoescapology: progress toward understanding the endosomal escape of polymeric nanoparticles. WIREs Nanomed. Nanobiotechnol. 9, e1452 (2017).
Olden, B. R., Cheng, Y., Yu, J. L. & Pun, S. H. Cationic polymers for non-viral gene delivery to human T cells. J. Control. Release 282, 140–147 (2018).
Prazeres, P. H. D. M. et al. Delivery of plasmid DNA by ionizable lipid nanoparticles to induce CAR expression in T cells. Int. J. Nanomed. 18, 5891–5904 (2023).
Billingsley, M. M. et al. Ionizable lipid nanoparticle-mediated mRNA delivery for human CAR T cell engineering. Nano Lett. 20, 1578–1589 (2020).
Padilla, M. S. et al. Branched endosomal disruptor (BEND) lipids mediate delivery of mRNA and CRISPR-Cas9 ribonucleoprotein complex for hepatic gene editing and T cell engineering. Nat. Commun. 16, 996 (2025).
Metzloff, A. E. et al. Antigen presenting cell mimetic lipid nanoparticles for rapid mRNA CAR T cell cancer immunotherapy. Adv. Mater. 36, 2313226 (2024). This publication presents lipid nanoparticles conjugated with anti-CD3 and anti-CD28, and encapsulating CAR mRNA, enabling activation and transfection of primary human T cells in a single step.
Billingsley, M. M. et al. Orthogonal design of experiments for optimization of lipid nanoparticles for mRNA engineering of CAR T cells. Nano Lett. 22, 533–542 (2022).
Yee Mon, K. J. et al. Functionalized nanowires for miRNA-mediated therapeutic programming of naïve T cells. Nat. Nanotech. 19, 1190–1202 (2024).
Hamilton, A. G. et al. Ionizable lipid nanoparticles with integrated immune checkpoint inhibition for mRNA CAR T cell engineering. Adv. Healthc. Mater. 12, 2301515 (2023).
Chamberlain, C. A. et al. Highly efficient PD-1-targeted CRISPR-Cas9 for tumor-infiltrating lymphocyte-based adoptive T cell therapy. Mol. Ther. Oncolytics 24, 417–428 (2022).
Brudno, J. N., Maus, M. V. & Hinrichs, C. S. CAR T cells and T-cell therapies for cancer: a translational science review. JAMA 22, 1924–1935 (2024).
Wang, L. et al. The dilemmas and possible solutions for CAR-T cell therapy application in solid tumors. Cancer Lett. 591, 216871 (2024).
Zhang, A. Q. et al. Universal redirection of CAR T cells against solid tumours via membrane-inserted ligands for the CAR. Nat. Biomed. Eng. 7, 1113–1128 (2023).
Reinhard, K. et al. An RNA vaccine drives expansion and efficacy of claudin-CAR-T cells against solid tumors. Science 367, 446–453 (2020).
Yoon, J., Fagan, E., Jeong, M. & Park, J.-H. In situ tumor-infiltrating lymphocyte therapy by local delivery of an mRNA encoding membrane-anchored anti-CD3 single-chain variable fragment. ACS Nano 18, 32401–32420 (2024). This work explores the use of mRNA-loaded lipid nanoparticles in tumours, enabling the in vivo engineering of TAMs and tumour cells to express anti-CD3 and thereby promote in situ engagement of TILs.
Stephan, M. T., Moon, J. J., Um, S. H., Bersthteyn, A. & Irvine, D. J. Therapeutic cell engineering with surface-conjugated synthetic nanoparticles. Nat. Med. 16, 1035–1041 (2010).
Tang, L. et al. Enhancing T cell therapy through TCR-signaling-responsive nanoparticle drug delivery. Nat. Biotechnol. 36, 707–716 (2018).
Luo, Y. et al. IL-12 nanochaperone-engineered CAR T cell for robust tumor-immunotherapy. Biomaterials 281, 121341 (2022).
Liu, Y. et al. Cytokine conjugation to enhance T cell therapy. Proc. Natl Acad. Sci. USA 120, e2213222120 (2023).
Zheng, Y. et al. In vivo targeting of adoptively transferred T-cells with antibody- and cytokine-conjugated liposomes. J. Control. Release 172, 426–435 (2013).
Weiss, L. et al. Direct in vivo activation of T cells with nanosized immunofilaments inhibits tumor growth and metastasis. ACS Nano 17, 12101–12117 (2023).
Sun, Y. et al. DNA origami–based artificial antigen-presenting cells for adoptive T cell therapy. Sci. Adv. 8, eadd1106 (2022).
Meyer, R. A. et al. Biodegradable nanoellipsoidal artificial antigen presenting cells for antigen specific T-cell activation. Small 11, 1519 (2015).
Li, X. et al. Enhancing adoptive cell therapy by T cell loading of SHP2 inhibitor nanocrystals before infusion. ACS Nano 16, 10918–10930 (2022).
Stephan, M. T., Stephan, S. B., Bak, P., Chen, J. & Irvine, D. J. Synapse-directed delivery of immunomodulators using T-cell-conjugated nanoparticles. Biomaterials 33, 5776–5787 (2012).
Siriwon, N. et al. CAR-T cells surface-engineered with drug-encapsulated nanoparticles can ameliorate intratumoral T-cell hypofunction. Cancer Immunol. Res. 6, 812–824 (2018).
Chen, Z. et al. Nanoengineered CAR-T biohybrids for solid tumor immunotherapy with microenvironment photothermal-remodeling strategy. Small 17, 2007494 (2021).
Zhao, Z. et al. A collagenase nanogel backpack improves CAR-T cell therapy outcomes in pancreatic cancer. Nat. Nanotechnol. https://doi.org/10.1038/s41565-025-01924-1 (2025).
Nie, W. et al. Magnetic nanoclusters armed with responsive PD-1 antibody synergistically improved adoptive T-cell therapy for solid tumors. ACS Nano 13, 1469–1478 (2019).
Schmid, D. et al. T cell-targeting nanoparticles focus delivery of immunotherapy to improve antitumor immunity. Nat. Commun. 8, 1747 (2017).
Zhang, F. et al. Nanoparticles that reshape the tumor milieu create a therapeutic window for effective T-cell therapy in solid malignancies. Cancer Res. 78, 3718–3730 (2018).
Chen, X. et al. Non-invasive activation of intratumoural gene editing for improved adoptive T-cell therapy in solid tumours. Nat. Nanotechnol. 18, 933–944 (2023). This article presents a mild heat-activated Cas9-based nanodevice that simultaneously disrupts immunosuppression in the tumour microenvironment and the apoptotic resistance of tumour cells, enhancing the infiltration and efficacy of TILs and CAR T cells.
Zhu, T. et al. Inhalable nanovesicles loaded with a STING agonist enhance CAR-T cell activity against solid tumors in the lung. Nat. Commun. 16, 262 (2025).
An, J., Guo, R., Liu, M., Hu, H. & Zhang, H. Multi-modal Ca2+ nanogenerator via reversing T cell exhaustion for enhanced chemo-immunotherapy. J. Control. Release 372, 715–727 (2024).
Miller, I. C. et al. Enhanced intratumoural activity of CAR T cells engineered to produce immunomodulators under photothermal control. Nat. Biomed. Eng. 5, 1348–1359 (2021).
Nguyen, N. T. et al. Nano-optogenetic engineering of CAR T cells for precision immunotherapy with enhanced safety. Nat. Nanotechnol. 16, 1424–1434 (2021).
Pfister, F. et al. Loading of CAR-T cells with magnetic nanoparticles for controlled targeting suppresses inflammatory cytokine release and switches tumor cell death mechanism. MedComm 6, e70039 (2025).
Gong, N. et al. In situ PEGylation of CAR T cells alleviates cytokine release syndrome and neurotoxicity. Nat. Mater. 22, 1571–1580 (2023).
Short, L., Holt, R. A., Cullis, P. R. & Evgin, L. Direct in vivo CAR T cell engineering. Trends Pharmacol. Sci. 45, 406–418 (2024).
Smith, T. T. et al. In situ programming of leukaemia-specific T cells using synthetic DNA nanocarriers. Nat. Nanotechnol. 12, 813–820 (2017).
Zhu, C. et al. Injectable supramolecular hydrogels for in situ programming of CAR-T cells toward solid tumor immunotherapy. Adv. Mater. 36, 2310078 (2024).
Zhou, J. E. et al. Lipid nanoparticles produce chimeric antigen receptor T cells with interleukin-6 knockdown in vivo. J. Control. Release 350, 298–307 (2022).
Parayath, N. N., Stephan, S. B., Koehne, A. L., Nelson, P. S. & Stephan, M. T. In vitro-transcribed antigen receptor mRNA nanocarriers for transient expression in circulating T cells in vivo. Nat. Commun. 11, 6080 (2020). This study explores mRNA-loaded polymer nanocarriers that programme host T cells to transiently express tumour-specific CARs directly in vivo.
Billingsley, M. M. et al. In vivo mRNA CAR T cell engineering via targeted ionizable lipid nanoparticles with extrahepatic tropism. Small 20, 2304378 (2024).
Álvarez-Benedicto, E. et al. Spleen SORT LNP generated in situ CAR T cells extend survival in a mouse model of lymphoreplete B cell lymphoma. Angew. Chem. Int. Ed. 62, e202310395 (2023).
Zhao, G., Zhang, Y., Xu, C. F. & Wang, J. In vivo production of CAR-T cells using virus-mimetic fusogenic nanovesicles. Sci. Bull. 69, 354–366 (2024).
Hamilton, E. et al. 801PRIMETM IL-15 (RPTR-147): preliminary clinical results and biomarker analysis from a first-in-human Phase 1 study of IL-15 loaded peripherally-derived autologous T cell therapy in solid tumor patients. J. Immunother. Cancer 8, A479–A480 (2020).
Amor, C. et al. Senolytic CAR T cells reverse senescence-associated pathologies. Nature 583, 127–132 (2020).
Seif, M. et al. CAR T cells targeting Aspergillus fumigatus are effective at treating invasive pulmonary aspergillosis in preclinical models. Sci. Transl. Med. 14, eabh1209 (2022).
Mackensen, A. et al. Anti-CD19 CAR T cell therapy for refractory systemic lupus erythematosus. Nat. Med. 28, 2124–2132 (2022).
Lidar, M. et al. CD-19 CAR-T cells for polyrefractory rheumatoid arthritis. Ann. Rheum. Dis. 84, 370–372 (2024).
Mohammadi, V. et al. Chimeric antigen receptor (CAR)-based cell therapy for type 1 diabetes mellitus (T1DM); current progress and future approaches. Stem. Cell. Rev. Rep. 20, 585–600 (2024).
Rurik, J. G. et al. CAR T cells produced in vivo to treat cardiac injury. Science 375, 91–96 (2022).
Qasim, W. et al. Molecular remission of infant B-ALL after infusion of universal TALEN gene-edited CAR T cells. Sci. Transl. Med. 9, eaaj2013 (2017).
Schaible, P., Bethge, W., Lengerke, C. & Haraszti, R. A. RNA therapeutics for improving CAR T-cell safety and efficacy. Cancer Res. 83, 354–362 (2023).
Themeli, M. et al. Generation of tumor-targeted human T lymphocytes from induced pluripotent stem cells for cancer therapy. Nat. Biotechnol. 31, 928–933 (2013).
Jing, R. et al. EZH1 repression generates mature iPSC-derived CAR T cells with enhanced antitumor activity. Cell Stem Cell 29, 1181–1196.E6 (2022).
Makkouk, A. et al. Off-the-shelf Vδ1 gamma delta T cells engineered with glypican-3 (GPC-3)-specific chimeric antigen receptor (CAR) and soluble IL-15 display robust antitumor efficacy against hepatocellular carcinoma. J. Immunother. Cancer 9, e003441 (2021).
Liu, E. et al. Use of CAR-Transduced natural killer cells in CD19-positive lymphoid tumors. N. Engl. J. Med. 382, 545–553 (2020).
Hudson, D., Fernandes, R. A., Basham, M., Ogg, G. & Koohy, H. Can we predict T cell specificity with digital biology and machine learning? Nat. Rev. Immunol. 23, 511–521 (2023). This perspective article explores how integrating digital biology with machine learning can enhance the prediction of TCR–antigen specificity, deepening our understanding of antigen immunogenicity and informing the development of CAR T and TIL therapies.
Zhang, D. K. Y. et al. Enhancing CAR-T cell functionality in a patient-specific manner. Nat. Commun. 14, 506 (2023).
Daniels, K. G. et al. Decoding CAR T cell phenotype using combinatorial signaling motif libraries and machine learning. Science 378, 1194–1200 (2022).
Bogatu, A. et al. Meta-analysis informed machine learning: Supporting cytokine storm detection during CAR-T cell Therapy. J. Biomed. Inform. 142, 104367 (2023).
Arabi, F., Mansouri, V. & Ahmadbeigi, N. Gene therapy clinical trials, where do we go? An overview. Biomed. Pharmacother. 153, 113324 (2022).
Moradi, V., Omidkhoda, A. & Ahmadbeigi, N. The paths and challenges of ‘off-the-shelf’ CAR-T cell therapy: an overview of clinical trials. Biomed. Pharmacother. 169, 115888 (2023).
Pfeiffer, A. et al. In vivo generation of human CD 19‐ CAR T cells results in B‐cell depletion and signs of cytokine release syndrome. EMBO Mol. Med. 10, e9158 (2018).
Agarwal, S., Weidner, T., Thalheimer, F. B. & Buchholz, C. J. In vivo generated human CAR T cells eradicate tumor cells. Oncoimmunology 8, e1671761 (2019).
Agarwal, S. et al. In vivo generation of CAR T cells selectively in human CD4+ lymphocytes. Mol. Ther. 28, 1783–1794 (2020).
Frank, A. M. et al. Combining T-cell–specific activation and in vivo gene delivery through CD3-targeted lentiviral vectors. Blood Adv. 4, 5702–5715 (2020).
Nicolai, C. J. et al. In vivo CAR T-cell generation in nonhuman primates using lentiviral vectors displaying a multidomain fusion ligand. Blood 144, 977–987 (2024).
Michels, K. R. et al. Preclinical proof of concept for VivoVec, a lentiviral-based platform for in vivo CAR T-cell engineering. J. Immunother. Cancer 11, e006292 (2023).
Huckaby, J. T. et al. Bispecific binder redirected lentiviral vector enables in vivo engineering of CAR-T cells. J. Immunother. Cancer 9, e002737 (2021).
Nawaz, W. et al. AAV-mediated in vivo CAR gene therapy for targeting human T-cell leukemia. Blood Cancer J. 11, 119 (2021).
Jeffreys, N., Brockman, J. M., Zhai, Y., Ingber, D. E. & Mooney, D. J. Mechanical forces amplify TCR mechanotransduction in T cell activation and function. Appl. Phys. Rev. 11, 011304 (2024).
Li, R., Ma, C., Cai, H. & Chen, W. The CAR T-cell mechanoimmunology at a glance. Adv. Sci. 7, 2002628 (2020).
Chow, A., Perica, K., Klebanoff, C. A. & Wolchok, J. D. Clinical implications of T cell exhaustion for cancer immunotherapy. Nat. Rev. Clin. Oncol. 19, 775–790 (2022).
Yin, X., He, L. & Guo, Z. T-cell exhaustion in CAR-T-cell therapy and strategies to overcome it. Immunology 169, 400–411 (2023).
Rafiq, S., Hackett, C. S. & Brentjens, R. J. Engineering strategies to overcome the current roadblocks in CAR T cell therapy. Nat. Rev. Clin. Oncol. 17, 147–167 (2019).
Norelli, M. et al. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat. Med. 24, 739–748 (2018).
Hughes, A. D., Teachey, D. T. & Diorio, C. Riding the storm: managing cytokine-related toxicities in CAR-T cell therapy. Semin. Immunopathol. 46, 1–19 (2024).