Weight-loss and diabetes drugs like GLP-1 receptor agonists have reshaped the treatment landscape, but they come with a catch: frequent injections to maintain their effects. Now, researchers in Japan have taken a striking step toward rewriting this paradigm by turning the liver into a long-term GLP-1 producer.
In a study titled “Targeted In Vivo Gene Integration of a Secretion-Enabled GLP-1 Receptor Agonist Reverses Diet-induced Non-genetic Obesity and Pre-diabetes,” and published in

Communications Medicine, scientists at the University of Osaka reported using a single genome editing treatment to engineer mice to produce their own supply of Exendin-4, a GLP-1 receptor agonist that controls appetite and blood sugar. The approach led to reduced food intake, attenuated weight gain, and improved metabolic health and insulin sensitivity in diet-induced obesity mouse models without any detectable adverse effects, the researchers reported.
“In vivo genome editing offers a long-term therapeutic approach for monogenic diseases by directly modifying genetic sequences,” the researchers wrote. “However, its application to non-monogenic, noncommunicable diseases…remains limited due to the lack of well-defined genetic targets.”
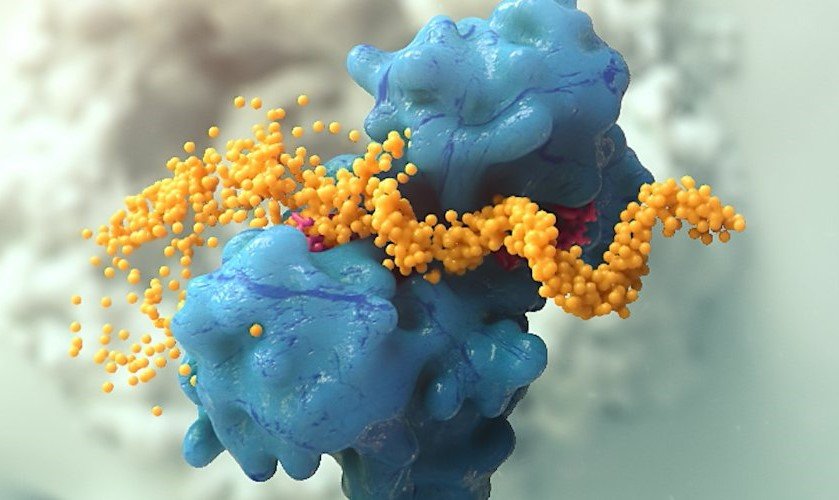
They explained that conventional homology-directed repair (HDR) is widely recognized as the most effective knock-in method for monogenic diseases. However, its reliance on cell division limits its use to proliferating tissues, excluding those with low cell turnover. To tackle this, the team pivoted from fixing faulty genes to installing entirely new ones. They used a homology-independent targeted integration (HITI) strategy—previously developed by the group—to insert a secretion-enabled version of the Exendin-4 gene into the Albumin locus of liver cells. The team chose this locus hepatocyte-specific high expression levels, ensuring robust and sustained secretion-enabled Exe4 (scExe4) peptide production.
Key to the delivery was the use of lipid nanoparticles (LNPs). The LNPs encapsulated plasmids encoding CRISPR-Cas9, guide RNAs, and the engineered Exendin-4 gene, allowing efficient targeting of the liver while minimizing off-target effects elsewhere.
Plasma Exendin-4 levels remained elevated in treated mice for more than 28 weeks following a single administration. ELISA assays confirmed persistent secretion of the peptide from the liver. Functionally, these mice had a 29% decrease in food intake and a 34% decrease in body weight. They also showed improved glucose tolerance and insulin sensitivity compared to untreated controls. Blood HbA1c and insulin levels also improved, mirroring profiles seen in lean mice.
Importantly, the researchers reported that next-generation sequencing and 5’-RACE analyses revealed minimal off-target effects, and liver enzymes remained within normal ranges. The approach also preserved the natural regulation of other hormones like GLP-1.
“This study demonstrates that a single administration of genome editing can achieve sustained therapeutic peptide secretion, providing a potential strategy for treating complex diseases without defined genetic causes,” the authors concluded.
While the work is still preclinical, it hints at a potential future: treating chronic, multifactorial conditions like obesity and type II diabetes with a one-time genetic intervention that turns the patient’s own cells into long-term producers of therapeutic biologics. The team also highlighted the possibility of fine-tuning this approach through repeat administrations, thanks to the nature of LNPs.
With further refinements—potentially using mRNA to avoid lingering Cas9 DNA—this strategy could extend beyond metabolic diseases to conditions like chronic inflammation or neurodegeneration, fundamentally reshaping how we think about biologics.
The post Obesity Reversed in Genome Edited Mice that Produce Their Own GLP-1 appeared first on GEN – Genetic Engineering and Biotechnology News.