Phase I clinical trial results suggest that an antibody treatment, used in combination with other drugs, enabled stem cell transplants for three children with Fanconi anemia without toxic busulfan chemotherapy or radiation. All three children with Fanconi anemia—a genetic disease that makes standard stem cell transplant extremely risky—have completed two years of follow-up and are doing well.
“We were able to treat these really fragile patients with a new, innovative regimen that allowed us to reduce the toxicity of the stem cell transplant protocol,” said Agnieszka Czechowicz, MD, PhD, assistant professor of pediatrics at Stanford Medicine. “Specifically, we could eliminate the use of radiation and genotoxic chemotherapy called busulfan, with exceptional outcomes.”
The results of the clinical trial were published in Nature Medicine in the paper, “Irradiation- and busulfan-free stem cell transplantation in Fanconi anemia using an anti-CD117 antibody: a Phase Ib trial.”
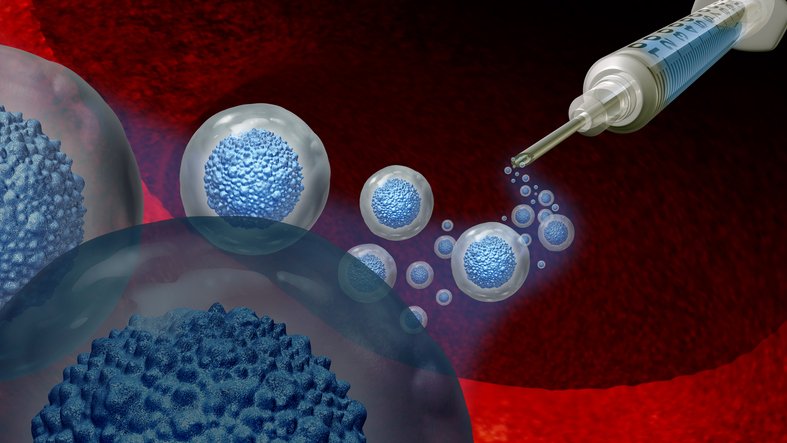
Before undergoing a stem cell transplant, a patient’s own stem cells must be eliminated, typically with radiation or chemotherapy. In this trial, patients were instead injected with antibodies against CD117, a protein on the surface of blood-forming stem cells. The antibody, briquilimab, eliminates blood-forming stem cells without toxic side effects.
One consequence of Fanconi anemia, which interferes with DNA repair, is impaired development of blood cells, including oxygen-carrying red blood cells; white blood cells needed for immune function; and platelets. Patients experience fatigue, reduced growth, frequent infections, and more bruising and bleeding than normal. Eventually, their blood cell production is so diminished they have the life-threatening condition of progressive bone marrow failure, signs of which develop in about 80% of Fanconi anemia patients by age 12.
Although a stem cell transplant can prevent and treat bone marrow failure in children with Fanconi anemia, patients are extremely vulnerable to side effects—including cancer—from the chemotherapy or radiation used to prepare for these transplants because their DNA-repair machinery works so poorly.
“Right now, nearly all of these patients get secondary cancers by the time they’re 40,” Czechowicz said, adding that her team hopes their new approach will reduce those rates. Fanconi anemia patients are also more vulnerable than other people to complications of graft-versus-host disease.
The three trial participants were all younger than 10 when they received their transplants. They were of different racial/ethnic backgrounds and had different gene mutations underlying their Fanconi anemia. Each patient received a single intravenous infusion of the antibody 12 days before they were scheduled to receive donated stem cells. Closer to the transplant date, they received immune-suppressing medications typically given before stem cell transplant, but no radiation or busulfan chemotherapy that is typically part of the treatment regimen.
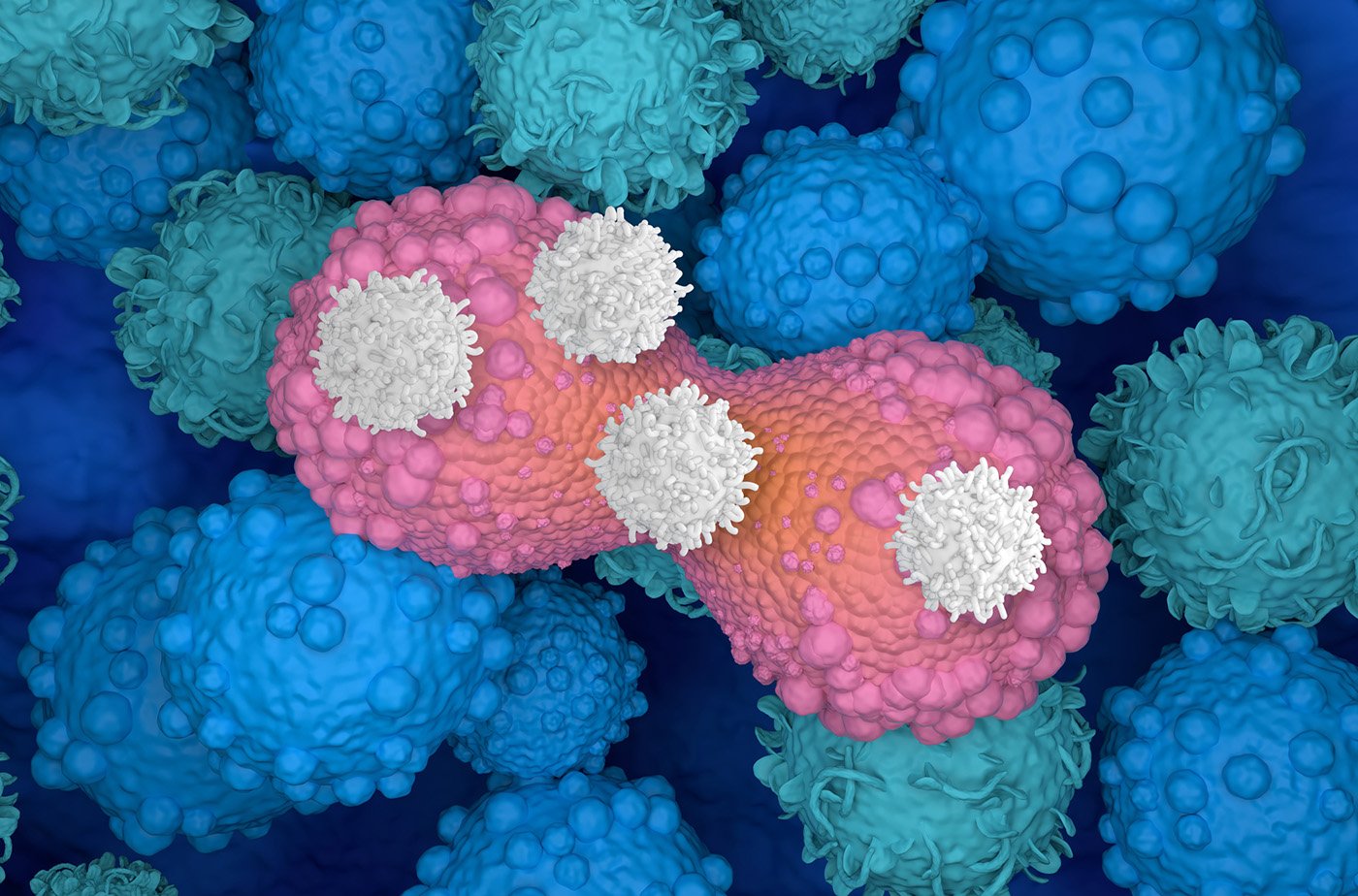
Each patient was then given a stem cell transplant consisting of cells that had been donated by a parent, depleted of alpha/beta T-cells and enriched for blood-forming stem cells. Within two weeks, the donated stem cells quickly took up residence in the patients’ bone marrow. No one experienced graft rejection and by 30 days after transplant, the healthy cells from the donors had almost completely taken over the patients’ marrow.
The researchers’ initial goal was to help patients reach 1% donor chimerism, meaning 1% of the bone marrow cells would come from the donor. But two years later, all three patients have close to 100% of their cells from their donors—far better than the researchers expected.
“We’ve been surprised by how well it’s worked,” Czechowicz said. “We were optimistic that we would get here, but you never know when you’re trying a new regimen.”
The clinical trial also addressed a second challenge in stem cell transplant. In the past, 35% to 40% of patients who needed transplants did not receive them because they lacked fully matched donors. But researchers found a way to increase the chance that the transplants would work by enriching for CD34+ cells—the donor’s blood-forming stem cells—by specifically removing alpha/beta T cells. The innovation reduces the risk of graft-versus-host disease, in which immune cells in donated bone marrow attack the recipient, and allows patients to receive cells from someone who shares only half of their immune markers (such as a parent).
“We are expanding the donors for stem cell transplantation in a major way, so every patient who needs a transplant can get one,” said Rajni Agarwal, MD, professor of pediatric stem cell transplantation at Stanford Medicine.
The researchers are now conducting a Phase II trial of the same protocol in additional children with Fanconi anemia. They also plan studies to test whether the new approach will work for other conditions, including Diamond-Blackfan anemia, another genetic disease that causes bone marrow failure. The group is also working on next-generation approaches that may continue to improve the treatment regimen for patients with Fanconi anemia as well as other grievous diseases.
The post Novel, Less Toxic, Stem Cell Transplant Prep Yields Successful Outcomes appeared first on GEN – Genetic Engineering and Biotechnology News.