Researchers headed by a team at Keck Medicine of USC have found that corticosteroids, which are commonly prescribed to non-small cell lung cancer (NSCLC) patients to alleviate cancer-related symptoms, may be responsible for the failure of some types of immunotherapy used to treat the disease.
The team’s study, headed by Keck Medicine oncologist and immunologist Fumito Ito, MD, PhD, evaluated the clinical outcomes of more than 250 patients with NSCLC receiving immune checkpoint inhibitor (ICI) therapy. The results showed that when compared with patients who were not receiving steroids, those patients given high doses of steroids before and/or during immunotherapy exhibited less tumor shrinkage, and also did not live as long.
“Steroids were the biggest predictor of why certain immunotherapies may not be effective, even when considering multiple other factors such as stage and progression of the disease,” said Ito. Additionally, the researchers believe they have found the mechanism behind why steroids and some immunotherapies may not mix. “Our findings reveal that steroids stop the body’s natural cancer-fighting cells, T cells, from maturing,” added Ito, who is a member and co-leader of the translational and clinical sciences research program at USC Norris Comprehensive Cancer Center. “This makes them unable to attack the cancer as vigorously as they usually would, leading to worse outcomes for patients. While other research has indicated steroids may negatively impact immunotherapy’s efficacy, we are one of the first to pinpoint a probable cause and effect.”
Ito is lead author of the team’s published paper in Cancer Research Communications, titled “Impact of Glucocorticoids on Immune Checkpoint Inhibitor Efficacy and Circulating Biomarkers in Non–Small Cell Lung Cancer Patients.”
“Immune checkpoint inhibitor (ICI) therapy has been revolutionary for patients with non–small cell lung cancer (NSCLC) …” the authors wrote. ICIs help the body’s immune system fight cancer by blocking proteins that prevent T cells from attacking cancer cells, and are often used to treat NSCLC, the most common form of lung cancer.
Steroids are commonly prescribed to alleviate symptoms of the cancer or treatments given for a variety of reasons, such as fatigue and vomiting, or more serious side effects such as brain swelling and lung inflammation. Steroids suppress the immune system, which reduces the inflammation that can cause these conditions. But as the authors also noted, while corticosteroids are frequently prescribed to patients with NSCLC for palliation of cancer-related symptoms, “… the potential impact of baseline steroid use on immune checkpoint inhibitor (ICI) therapy and its underlying mechanisms remain unclear.”
To examine the effect of steroids on immune checkpoint inhibitor therapy Ito and colleagues retrospectively studied the medical records of 277 patients with Stage II-IV NSCLC who were treated with ICIs alone or in combination with other therapies, at sites including USC Norris Comprehensive Cancer Center. “Here, we evaluate the impact of baseline steroid use on clinical outcomes and blood-based predictive correlates of response to ICI therapy in patients with NSCLC using independent cohorts from two academic institutions,” they wrote. Twenty-one patients (8%) were taking steroids at the start of ICIs. All 21 patients remained on steroids for at least 12 weeks after starting ICI therapy.
The team compared outcomes—tumor shrinkage and survival rate—between patients prescribed steroids and those who were not. An analysis of up to eight years of data indicated that steroids were the sole factor impeding the effectiveness of the immunotherapy. “Patients on baseline steroids had a lower overall response rate with markedly shorter progression-free survival and overall survival compared with those not receiving steroids,” the investigators reported. “In multivariate analysis, steroid use was the only significant independent risk factor for disease progression and mortality in both independent cohorts …”
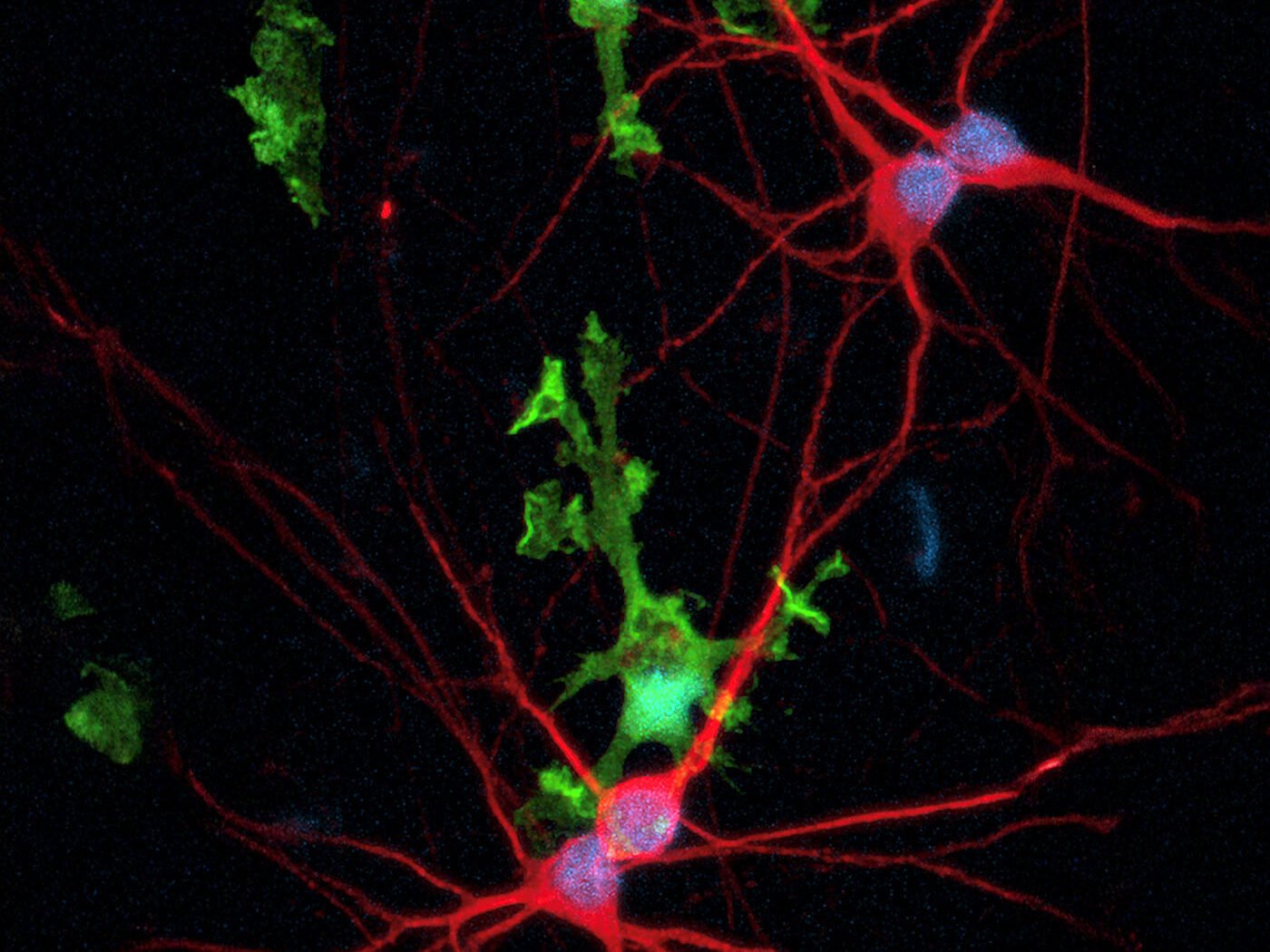
The team also discovered that the T cells of significant numbers of patients on steroids were not fully matured. “Additionally, the baseline frequency of circulating CX3CR1+CD8+ T cells was substantially lower in patients on steroids,” they stated. “Collectively, baseline steroid use was associated with worse outcomes and decreased frequency of circulating differentiated effector T cells in patients with NSCLC.”
Taking what they describe as a “bedside to bench” approach the team also carried out a preclinical study in mice to follow the effects of steroids on ICI therapy in real time. They treated mice bearing MC38 colon adenocarcinoma with anti–PD-L1 therapy in the absence or presence of dexamethasone, which was continued throughout or discontinued at the time of starting the anti-PD-L1 immunotherapy. The results showed that steroids given to the mice before/during immunotherapy inhibit T cells from fully maturing. “We found that pre- and on-treatment steroid administration substantially decreased antitumor efficacy of anti–PD-L1 therapy and survival. However, we did not observe the negative impact of dexamethasone when it was discontinued at the time of initiation of anti–PD-L1 therapy.”
The scientists also discovered that steroids blocked biomarkers circulating in the bloodstream that signal when cancer is progressing so oncologists can adjust the patient’s treatment, writing, “Systemic effects of steroids complicate the interpretation of predictive blood-based biomarkers such as NLR and the CX3CR1 score, reducing their prognostic value.” Ito further noted, “Without the presence of circulating biomarkers to inform our decisions, oncologists cannot treat the cancer as effectively and patients may miss out on the best treatment for their cancer.”
The authors added in summary, “This study shows that baseline steroid use is a negative independent prognostic factor in patients with NSCLC undergoing ICI therapy and provides insights into the decreased T-cell effector differentiation and utility of predictive blood-based markers by steroids.”
While the Keck Medicine research indicates steroids can be harmful to ICI therapy, Ito acknowledges that for some patients, steroids may be necessary to manage their cancer-related symptoms. “Treating cancer is a balancing act between fighting the cancer with effective therapies while addressing the patient’s quality of life,” Ito pointed out. “We believe there is room for steroids during immunotherapy, but it is important to understand their potential limitations.”
Ito hopes the research will lead to additional studies examining the effect of steroids on immunotherapy so oncologists can make fully informed decisions that will best benefit their patients.
The post Corticosteroids Reduce Effectiveness of Immunotherapy for NSCLC appeared first on GEN – Genetic Engineering and Biotechnology News.