Cutting off blood flow can prematurely age the bone marrow, weakening the immune system’s ability to fight cancer, according to a new study from NYU Langone Health.
The team’s preclinical study showed that peripheral ischemia—restricted blood flow in the arteries in the legs—caused breast tumors in mice to grow at double the rate seen in mice without restricted flow. The findings build on a 2020 study from the same team, which reported ischemia during a heart attack to have the same effect.
“Our study shows that impaired blood flow drives cancer growth regardless of where it happens in the body,” says corresponding author Kathryn J. Moore, PhD, the Jean and David Blechman professor of cardiology in the department of medicine, Leon H. Charney division of cardiology, NYU Grossman School of Medicine. “This link between peripheral artery disease and breast cancer growth underscores the critical importance of addressing metabolic and vascular risk factors as part of a comprehensive cancer treatment strategy.”
Moore is senior and corresponding author of the team’s published paper in JACC CardioOncology, titled “Ischemic Injury Drives Nascent Tumor Growth via Accelerated Hematopoietic Aging.” In their report the team stated, “Peripheral ischemia enhances inflammaging of hematopoietic stem cells and long-lasting alterations to antitumoral immunity, accelerating breast tumor growth.”
Cardiovascular disease (CVD) and cancer are the two leading causes of death globally, and evidence increasingly suggests that these diseases share common risk factors and pathophysiological mechanisms, “resulting in bidirectional cross-disease communication,” the authors wrote. Epidemiological studies have shown that adult cancer survivors have increased risk of CVD, while individuals diagnosed with CVD have an increased risk of incident cancer and metastasis. “However, the intricacies of this detrimental relationship are not well defined,” the team continued. Interestingly, they noted, “Clinical findings suggest that myocardial infarction (MI), a common consequence of atherosclerotic CVD, can increase cancer risk and worsen outcomes in cancer patients.”
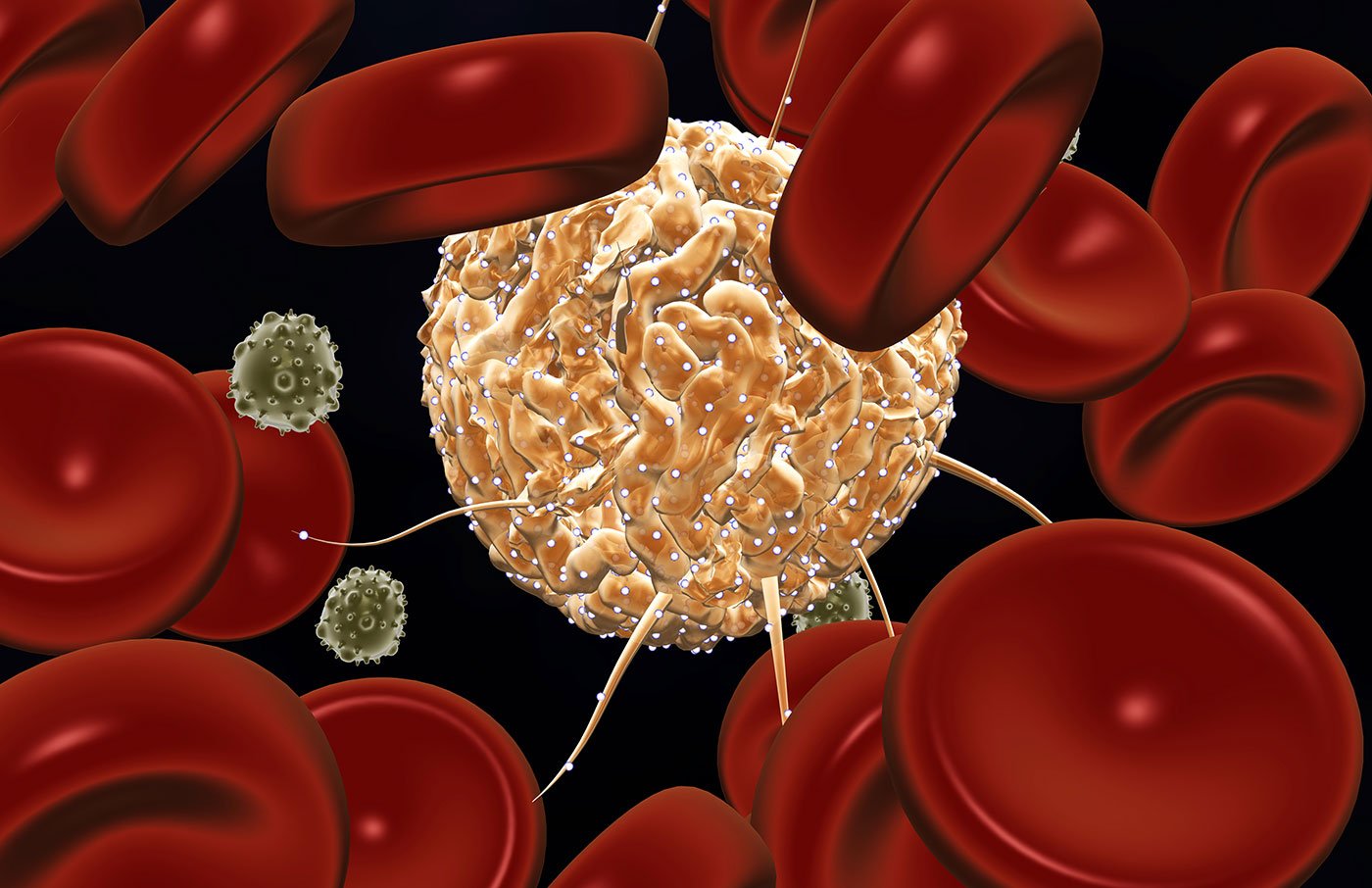
Ischemia occurs when fatty deposits, such as cholesterol, accumulate in artery walls, leading to inflammation and clotting that restrict the flow of oxygen-rich blood. When this happens in the legs, it causes peripheral artery disease, which affects millions of Americans, and can increase the risk of heart attack or stroke. To examine the mechanisms behind the link between cardiovascular disease and cancer growth, the study authors developed a mouse model with breast tumors and induced temporary ischemia in one hind limb (hind limb ischemia; HLI). The team then compared cancer growth in mice with and without impaired blood flow.
“Monitoring of tumor volume by caliper measurements revealed a greater than two-fold increase in tumor growth in HLI- compared with sham-treated mice,” they stated, and a doubling of tumor burden at the study endpoint, which was 21 days after surgery. “This degree of HLI-accelerated tumor growth was similar to what had been observed after coronary artery ligation in a mouse model of acute MI, suggesting that, like cardiac ischemia, peripheral ischemic injury accelerates tumor growth,” they stated.
Importantly, the research team found that restricted blood flow triggers a shift toward immune cell populations that cannot efficiently fight infections and cancer, mirroring changes seen with aging. Normally, the immune system responds to injury or infection by ramping up inflammation to eliminate threats, then scaling back to avoid harm to healthy tissue.
This balance is maintained by a mix of immune cells that either activate or suppress inflammation. The newly reported results indicated that reduced blood flow disrupts this equilibrium. It reprograms stem cells in the bone marrow to favor the production of “myeloid” immune cells (monocytes, macrophages, neutrophils) that dampen immune responses, while reducing output of lymphocytes like T cells that help to mount strong anti-tumor responses.
The local environment within tumors showed a similar shift, accumulating more immune-suppressive cells—including Ly6Chi monocytes, M2-like F4/80+ MHCIIlo macrophages, and regulatory T cells—that shield cancer from immune attack. “Together, these findings indicate peripheral ischemia contributes to myeloid enrichment and suggest an immunosuppressive microenvironment that encourages tumor progression,” the investigators stated.
Further experiments showed that these immune changes were long-lasting. Ischemia not only altered the expression of hundreds of genes, shifting immune cells into a more cancer-tolerant state, but also reorganized the structure of chromatin, making it harder for immune cells to activate genes involved in fighting cancer. “Thus, ischemia induces sustained rearrangement within the bone marrow niche that is ultimately associated with the promotion of nascent tumor growth.”
The findings build on the nature of the immune system, which evolved to attack invading bacteria and viruses, and under normal conditions, to detect and eliminate cancer cells. These protective functions rely on stem cell reserves in the bone marrow, which can be activated as needed to produce key white blood cell populations throughout life.
“Our results reveal a direct mechanism by which ischemia drives cancer growth, reprogramming stem cells in ways that resemble aging and promote immune tolerance,” says first author Alexandra Newman, PhD, a postdoctoral scholar in Moore’s lab. “These findings open the door to new strategies in cancer prevention and treatment, like earlier cancer screening for patients with peripheral artery disease and using inflammation-modulating therapies to counter these effects.”
In summary, the authors wrote, “These findings reveal that peripheral ischemic injury drives profound reprogramming of HSPC behavior—marked by inflammatory gene activation, skewed myeloid differentiation, and coordinated epigenetic remodeling—that may accelerate tumor progression…As a result, targeting inflammation may offer a promising therapeutic strategy at the intersection of cancer and CVD.”
Moving forward, the research team hopes to help design clinical studies that evaluate whether existing inflammation-targeted therapies can counter post-ischemic changes driving tumor growth. The team in addition suggested, “future studies should evaluate if anti-inflammatories abrogate postischemic hematopoietic changes driving tumor growth.”
The post Ischemia Drives Breast Cancer Growth in Mice by Weakening Immunity appeared first on GEN – Genetic Engineering and Biotechnology News.