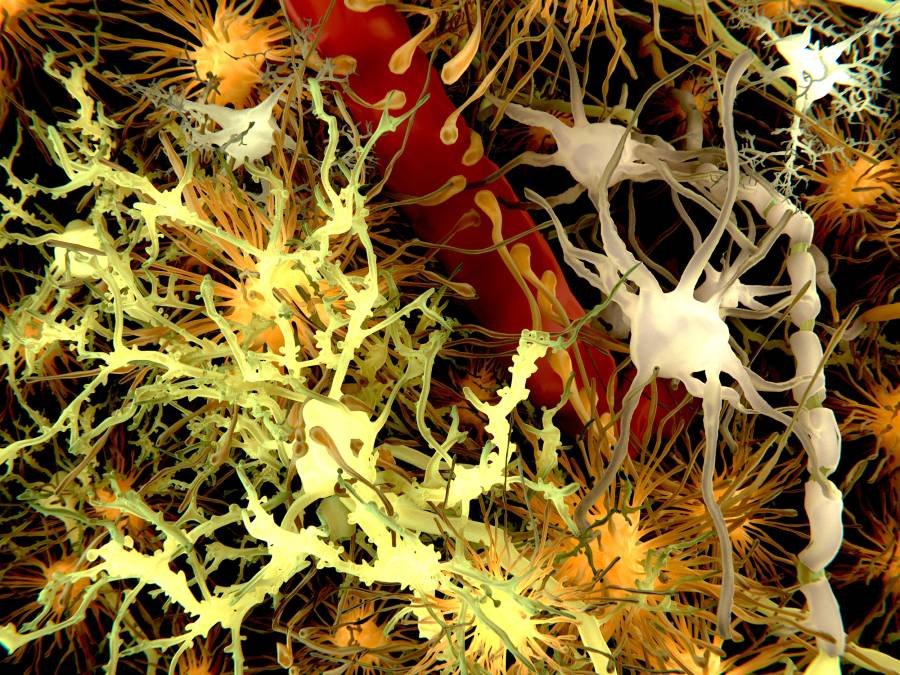
Genetic neurodegenerative disorders like Tay-Sachs and Sandhoff disease currently have no effective treatments. A possible strategy is replacing affected cells with healthy ones in order to slow the neurodegenerative process. But this approach is not without challenges, including poor engraftment in the brain and a graft-versus-host response.
Now scientists from Stanford University School of Medicine, University Hospital Hamburg-Eppendorf, and Research Institute Children’s Cancer Center Hamburg claim to have a strategy for replacing more than half of the most severely affected cells—specifically, microglia—with non-genetically matched precursor cells. If it is successful, their approach could be less damaging to patients than bone marrow transplants. Full details of their study in mice are published in a new Nature paper titled “Therapeutic genetic restoration through allogeneic brain microglia replacement.”**
According to Marius Wernig, MD, PhD, senior author on the study, pathology professor, and program leader at Stanford’s Institute for Stem Cell Biology and Regenerative Medicine, “we were able to achieve nearly 100% incorporation of genetically healthy cells in the brains of the mice while avoiding both rejection and graft-versus-host disease.” Furthermore, the treated mice not only survived for the duration of the experiment, but also had improved motor function and regained normal behaviors like exploring open spaces. “The difference between treated and control animals was dramatic.”
The mice used in the study had Sandhoff disease, which like Tay Sachs, is a lysosomal storage disorder. People with this rare condition lack the enzyme beta-hexosaminidase without which the lysosomes cannot function and fat builds up in cells, damaging the brain and other body systems. “Although the symptoms of these diseases are due to the degeneration of neurons, the levels of lysosomal enzymes in…microglia are sometimes a thousand-fold higher than in neurons,” Wernig said. So, why is it that the neurons are dying if the microglia are more severely affected?
One of the functions of microglia is to engulf and break down dead cells and pathogens in the brain. As a result, they need more degradative enzymes compared to other cells. This led the researchers to speculate that restoring lysosomal enzymes to the affected microglia could help slow the degeneration of neighboring neurons.
Earlier attempts to correct genetic deficiencies in microglia that are impacted in lysosomal storage disorders used bone marrow transplants to try to reboot the recipient’s immune infrastructure. But getting healthy cells into the brain is difficult because the body does an effective job of restricting access to the central nervous system. Other challenges include the risk of graft-versus-host disease and elimination of donor cells by lingering immune cells following preconditioning—the clearing of a host’s immune cells prior to a bone marrow transplant.
Previously, Wernig and his team showed that it was possible to achieve 90 percent engraftment of donor cells by wiping out the recipient’s immune system and killing off the microglia before transplanting them with donated stem cells. But that process is rough on patients, Wernig said. “It’s not something you want to do to your patients unless there’s no other option.”
And this is where the results reported in Nature come in.
Wernig and his team aimed to assess whether they could avoid the harsh effects of the preconditioning and stem cell transplant processes. To that end, they treated the mice with a microglia-depleting drug and irradiated their brains. They then injected microglia precursor cells from a non-genetically matched donor animal into the brains of the treatment mice. They then administered two drugs to block the activation of immune cells from elsewhere in the body.
When they analyzed the treated mice, the scientists found evidence of efficient engraftment of the donated cells in the brain. In fact, the cells developed into microglia without migrating to the rest of the body or being attacked by the recipient animal’s immune system. And the effect lasted for months post-treatment. According to the scientists, more than 85 percent of the microglial cells found in the brains eight months post transplantation were formed from the donated precursor cells.
Furthermore, untreated mice with a version of Sandhoff disease lived a median of 135 days and no animal lived beyond 155 days. In contrast, five of the animals treated with the brain-specific microglia transplantation therapy lived up to 250 days, when the experiment was terminated. Lastly, although the treated mice eventually developed hind leg paralysis, they displayed normal exploration behaviors in a large open pen and greater muscle strength and coordination than control animals.
The scientists also report an important finding about the lysosomal enzyme that mice with Sandhoff disease lack. When they explored the relationship between the donated microglia and neighboring neurons, they found that the missing lysosomal enzyme produced by the new microglia was present in the animals’ native neurons. Exactly how this is happening is not known. One possibility is that the microglia pack and secrete the enzyme into the space between cells, and from there it is imported into the neurons. “This could be an important, unrecognized role for microglia: to supply lysosomal factors to the environment including neurons,” Wernig said.
While this treatment approach works in mice, the real test would be whether it can be used in humans. If so, it could improve the symptoms of children born with conditions like Sandhoff disease. Wernig and his colleagues are optimistic because the individual steps of their treatment strategy are already used to treat other kinds of diseases. “We’ve solved three big problems with this study,” Wernig said. “We achieved efficient brain-restricted transplantation without systemic toxic preconditioning, we were able to use non-genetically matched cells that don’t require genetic engineering to make the missing lysosomal enzyme, and we avoided immune rejection and graft-versus-host disease.”
**Per Nature, the paper associated with this article was published unedited to give early access to its findings, with plans to publish an edited version at a later time.
The post Microglia Replacement Strategy Mitigates Rare Neurodegenerative Disease in Mice appeared first on GEN – Genetic Engineering and Biotechnology News.