Doudna, J. A. The promise and challenge of therapeutic genome editing. Nature 578, 229–236 (2020).
Frangoul, H. et al. Exagamglogene autotemcel for severe sickle cell disease. N. Engl. J. Med. 390, 1649–1662 (2024).
Locatelli, F. et al. Exagamglogene autotemcel for transfusion-dependent β-thalassemia. N. Engl. J. Med. 390, 1663–1676 (2024).
Ottaviano, G. et al. Phase 1 clinical trial of CRISPR-engineered CAR19 universal T cells for treatment of children with refractory B cell leukemia. Sci. Transl. Med. 14, eabq3010 (2022).
Hu, Y. et al. CRISPR/Cas9-engineered universal CD19/CD22 dual-targeted CAR-T cell therapy for relapsed/refractory B-cell acute lymphoblastic leukemia. Clin. Cancer Res. 27, 2764–2772 (2021).
Khoshandam, M., Soltaninejad, H., Hamidieh, A. A. & Hosseinkhani, S. CRISPR, CAR-T, and NK: current applications and future perspectives. Genes Dis. 11, 101121 (2024).
Maeder, M. L. et al. Development of a gene-editing approach to restore vision loss in Leber congenital amaurosis type 10. Nat. Med. 25, 229–233 (2019).
Sinha, D. et al. Human iPSC modeling reveals mutation-specific responses to gene therapy in a genotypically diverse dominant maculopathy. Am. J. Hum. Genet. 107, 278–292 (2020). This study directly compares gene editing with gene augmentation within patient-derived iPS cell retinal models.
Kabra, M. et al. Nonviral base editing of KCNJ13 mutation preserves vision in a model of inherited retinal channelopathy. J. Clin. Invest. 133, e171356 (2023).
Lee, R. G. et al. Efficacy and safety of an investigational single-course CRISPR base-editing therapy targeting PCSK9 in nonhuman primate and mouse models. Circulation 147, 242–253 (2023).
Nelson, C. E. et al. Long-term evaluation of AAV-CRISPR genome editing for Duchenne muscular dystrophy. Nat. Med. 25, 427–432 (2019).
Pickar-Oliver, A. et al. Full-length dystrophin restoration via targeted exon integration by AAV-CRISPR in a humanized mouse model of duchenne muscular dystrophy. Mol. Ther. 29, 3243–3257 (2021).
Gillmore, J. D. et al. CRISPR–Cas9 in vivo gene editing for transthyretin amyloidosis. N. Engl. J. Med. 385, 493–502 (2021).
Lek, A. et al. Death after high-dose rAAV9 gene therapy in a patient with Duchenne’s muscular dystrophy. N. Engl. J. Med. 389, 1203–1210 (2023).
Pierce, E. A. et al. Gene editing for CEP290-associated retinal degeneration. N. Engl. J. Med. 390, 1972–1984 (2024).
Longhurst, H. J. et al. CRISPR–Cas9 in vivo gene editing of KLKB1 for hereditary angioedema. N. Engl. J. Med. 390, 432–441 (2024).
Musunuru, K. et al. Patient-specific in vivo gene editing to treat a rare genetic disease. N. Engl. J. Med. 392, 2235–2243 (2025). This study describes the custom development and application of a gene-editing treatment to an infant with CPS1 deficiency within 8 months of diagnosis.
US FDA Center for Biologics Evaluation and Research (CEBR). Human gene therapy products incorporating human genome editing; https://www.fda.gov/regulatory-information/search-fda-guidance-documents/human-gene-therapy-products-incorporating-human-genome-editing (2024).
Torre, M. et al. Neuropathology of a case with fatal CAR T-cell-associated cerebral edema. J. Neuropathol. Exp. Neurol. 77, 877–882 (2018).
Anliker, B. et al. Regulatory considerations for clinical trial applications with CRISPR-based medicinal products. CRISPR J. 5, 364–376 (2022).
Adler, M. et al. A quantitative approach to screen for nephrotoxic compounds in vitro. J. Am. Soc. Nephrol. 27, 1015–1028 (2016).
Mitchell, T. J. et al. Timing the landmark events in the evolution of clear cell renal cell cancer: TRACERx Renal. Cell 173, 611–623.e17 (2018).
Mays, L. E. & Wilson, J. M. The complex and evolving story of T cell activation to AAV vector-encoded transgene products. Mol. Ther. 19, 16–27 (2011).
Chew, W. L. et al. A multifunctional AAV–CRISPR–Cas9 and its host response. Nat. Methods 13, 868–874 (2016).
Charlesworth, C. T. et al. Identification of preexisting adaptive immunity to Cas9 proteins in humans. Nat. Med. 25, 249–254 (2019).
Hakim, C. H. et al. Cas9-specific immune responses compromise local and systemic AAV CRISPR therapy in multiple dystrophic canine models. Nat. Commun. 12, 6769 (2021).
Hooper, A. J., Tang, X. L. & Burnett, J. R. VERVE-101, a CRISPR base-editing therapy designed to permanently inactivate hepatic PCSK9 and reduce LDL-cholesterol. Expert Opin. Investig. Drugs 33, 753–756 (2024).
van Haasteren, J., Li, J., Scheideler, O. J., Murthy, N. & Schaffer, D. V. The delivery challenge: fulfilling the promise of therapeutic genome editing. Nat. Biotechnol. 38, 845–855 (2020).
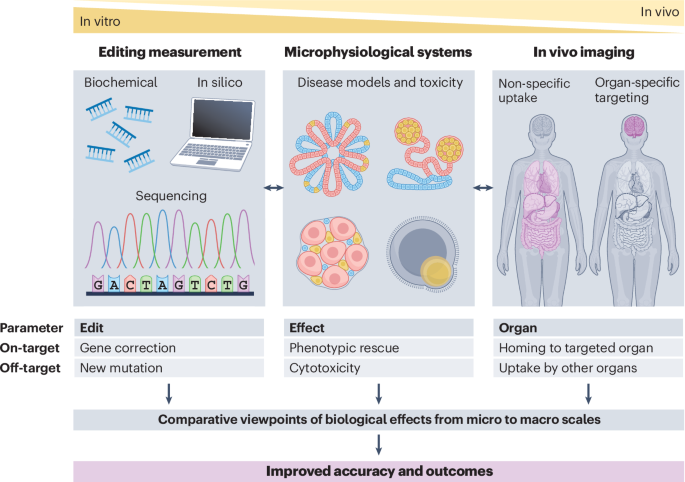
Saha, K. et al. The NIH Somatic Cell Genome Editing program. Nature 592, 195–204 (2021). This white paper describes the general goals and achievements of the SCGE Consortium during its first phase, including the development of a toolkit for data and protocol deposition.
Pacesa, M., Pelea, O. & Jinek, M. Past, present, and future of CRISPR genome editing technologies. Cell 187, 1076–1100 (2024).
Suchy, F. P. et al. Genome engineering with Cas9 and AAV repair templates generates frequent concatemeric insertions of viral vectors. Nat. Biotechnol. 43, 204–213 (2025).
Kosicki, M., Tomberg, K. & Bradley, A. Repair of double-strand breaks induced by CRISPR–Cas9 leads to large deletions and complex rearrangements. Nat. Biotechnol. 36, 765–771 (2018).
Fiumara, M. et al. Genotoxic effects of base and prime editing in human hematopoietic stem cells. Nat. Biotechnol. 42, 877–891 (2024).
Guschin, D. Y. et al. A rapid and general assay for monitoring endogenous gene modification. Methods Mol. Biol. 649, 247–256 (2010).
Mashal, R. D., Koontz, J. & Sklar, J. Detection of mutations by cleavage of DNA heteroduplexes with bacteriophage resolvases. Nat. Genet. 9, 177–183 (1995).
Yang, Z. et al. Fast and sensitive detection of indels induced by precise gene targeting. Nucleic Acids Res. 43, e59 (2015).
Sentmanat, M. F., Peters, S. T., Florian, C. P., Connelly, J. P. & Pruett-Miller, S. M. A survey of validation strategies for CRISPR–Cas9 editing. Sci. Rep. 8, 888 (2018).
Gupta, N., Zhang, K., Sabbisetti, V., Shu, J. & Morizane, R. AAV for gene therapy drives a nephrotoxic response via NFκB in kidney organoids. Signal Transduct. Target. Ther. 10, 252 (2025). Human safety and efficacy profiling in kidney organoids reveals that a commonly used viral delivery system induces mitigatable NFκB-mediated nephrotoxicity.
Mali, P. et al. RNA-guided human genome engineering via Cas9. Science 339, 823–826 (2013).
Certo, M. T. et al. Tracking genome engineering outcome at individual DNA breakpoints. Nat. Methods 8, 671–676 (2011).
Zhang, J. et al. A multiple-capillary electrophoresis system for small-scale DNA sequencing and analysis. Nucleic Acids Res. 27, e36 (1999).
Vishy, C. E. et al. Genetics of cystogenesis in base-edited human organoids reveal therapeutic strategies for polycystic kidney disease. Cell Stem Cell 31, 537–553.e5 (2024). This study presents innovative human organoids with clinically relevant, gene-edited nonsense mutations as a proof of concept for base-edited gene therapy in PKD.
Kluesner, M. G. et al. EditR: a method to quantify base editing from Sanger sequencing. CRISPR J. 1, 239–250 (2018).
Xu, L., Liu, Y. & Han, R. BEAT: a python program to quantify base editing from sanger sequencing. CRISPR J. 2, 223–229 (2019).
Zhidkov, I., Cohen, R., Geifman, N., Mishmar, D. & Rubin, E. CHILD: a new tool for detecting low-abundance insertions and deletions in standard sequence traces. Nucleic Acids Res. 39, e47 (2011).
Conant, D. et al. Inference of CRISPR edits from Sanger trace data. CRISPR J. 5, 123–130 (2022).
Brinkman, E. K., Chen, T., Amendola, M. & van Steensel, B. Easy quantitative assessment of genome editing by sequence trace decomposition. Nucleic Acids Res. 42, e168 (2014).
Cruz, N. M. et al. Modelling ciliopathy phenotypes in human tissues derived from pluripotent stem cells with genetically ablated cilia. Nat. Biomed. Eng. 6, 463–475 (2022).
Cruz, N. M. & Freedman, B. S. CRISPR gene editing in the kidney. Am. J. Kidney Dis. 71, 874–883 (2018).
Watry, H. L. et al. Rapid, precise quantification of large DNA excisions and inversions by ddPCR. Sci. Rep. 10, 14896 (2020).
Logsdon, G. A., Vollger, M. R. & Eichler, E. E. Long-read human genome sequencing and its applications. Nat. Rev. Genet. 21, 597–614 (2020).
Dua, P. H. et al. Haplotype editing with CRISPR/Cas9 as a therapeutic approach for dominant-negative missense mutations in NEFL. Preprint at bioRxiv https://doi.org/10.1101/2024.12.20.629813 (2024).
Mardis, E. R. & Wilson, R. K. Tracing the evolution of sequencing into the era of genomic medicine. Nat. Rev. Genet. 26, 719–734 (2025).
Giannoukos, G. et al. UDiTaSTM, a genome editing detection method for indels and genome rearrangements. BMC Genomics 19, 212 (2018).
Levene, M. J. et al. Zero-mode waveguides for single-molecule analysis at high concentrations. Science 299, 682–686 (2003).
Rang, F. J., Kloosterman, W. P. & de Ridder, J. From squiggle to basepair: computational approaches for improving nanopore sequencing read accuracy. Genome Biol. 19, 90 (2018).
Jain, M. et al. Nanopore sequencing and assembly of a human genome with ultra-long reads. Nat. Biotechnol. 36, 338–345 (2018).
Clarke, J. et al. Continuous base identification for single-molecule nanopore DNA sequencing. Nat. Nanotechnol. 4, 265–270 (2009).
Stergachis, A. B., Debo, B. M., Haugen, E., Churchman, L. S. & Stamatoyannopoulos, J. A. Single-molecule regulatory architectures captured by chromatin fiber sequencing. Science 368, 1449–1454 (2020).
Chen, Z. et al. DNA translocation through an array of kinked nanopores. Nat. Mater. 9, 667–675 (2010).
Chiba, K. et al. Mutations in the promoter of the telomerase gene TERT contribute to tumorigenesis by a two-step mechanism. Science 357, 1416–1420 (2017).
Ihry, R. J. et al. p53 inhibits CRISPR–Cas9 engineering in human pluripotent stem cells. Nat. Med. 24, 939–946 (2018).
Haapaniemi, E., Botla, S., Persson, J., Schmierer, B. & Taipale, J. CRISPR–Cas9 genome editing induces a p53-mediated DNA damage response. Nat. Med. 24, 927–930 (2018).
Harlander, S. et al. Combined mutation in Vhl, Trp53 and Rb1 causes clear cell renal cell carcinoma in mice. Nat. Med. 23, 869–877 (2017).
Hacein-Bey-Abina, S. et al. LMO2-associated clonal T cell proliferation in two patients after gene therapy for SCID-X1. Science 302, 415–419 (2003).
Cavazzana-Calvo, M. et al. Gene therapy of human severe combined immunodeficiency (SCID)-X1 disease. Science 288, 669–672 (2000).
Hacein-Bey-Abina, S. et al. Sustained correction of X-linked severe combined immunodeficiency by ex vivo gene therapy. N. Engl. J. Med. 346, 1185–1193 (2002).
Verdun, N. & Marks, P. Secondary cancers after chimeric antigen receptor T-cell therapy. N. Engl. J. Med. 390, 584–586 (2024).
Duncan, C. N. et al. Hematologic cancer after gene therapy for cerebral adrenoleukodystrophy. N. Engl. J. Med. 391, 1287–1301 (2024).
Sachdev, A. et al. Reversal of C9orf72 mutation-induced transcriptional dysregulation and pathology in cultured human neurons by allele-specific excision. Proc. Natl Acad. Sci. USA 121, e2307814121 (2024).
van den Berg, L. H. et al. Safety, tolerability, and pharmacokinetics of antisense oligonucleotide BIIB078 in adults with C9orf72-associated amyotrophic lateral sclerosis: a phase 1, randomised, double blinded, placebo-controlled, multiple ascending dose study. Lancet Neurol. 23, 901–912 (2024).
Sternberg, S. H., Redding, S., Jinek, M., Greene, E. C. & Doudna, J. A. DNA interrogation by the CRISPR RNA-guided endonuclease Cas9. Nature 507, 62–67 (2014).
Cradick, T. J., Qiu, P., Lee, C. M., Fine, E. J. & Bao, G. COSMID: A Web-based Tool for Identifying and Validating CRISPR/Cas Off-target Sites. Mol. Ther. Nucleic Acids 3, e214 (2014).
Stemmer, M., Thumberger, T., Del Sol Keyer, M., Wittbrodt, J. & Mateo, J. L. CCTop: an intuitive, flexible and reliable CRISPR/Cas9 target prediction tool. PLoS ONE 10, e0124633 (2015).
Bae, S., Park, J. & Kim, J.-S. Cas-OFFinder: a fast and versatile algorithm that searches for potential off-target sites of Cas9 RNA-guided endonucleases. Bioinformatics 30, 1473–1475 (2014).
Listgarten, J. et al. Prediction of off-target activities for the end-to-end design of CRISPR guide RNAs. Nat. Biomed. Eng. 2, 38–47 (2018).
Chuai, G. et al. DeepCRISPR: optimized CRISPR guide RNA design by deep learning. Genome Biol. 19, 80 (2018).
Aqil, M., Atasoy, S., Kringelbach, M. L. & Hindriks, R. Graph neural fields: a framework for spatiotemporal dynamical models on the human connectome. PLoS Comput. Biol. 17, e1008310 (2021).
Kim, D. et al. Digenome-seq: genome-wide profiling of CRISPR–Cas9 off-target effects in human cells. Nat. Methods 12, 237–243 (2015).
Cameron, P. et al. Mapping the genomic landscape of CRISPR–Cas9 cleavage. Nat. Methods 14, 600–606 (2017).
Tsai, S. Q. et al. CIRCLE-seq: a highly sensitive in vitro screen for genome-wide CRISPR–Cas9 nuclease off-targets. Nat. Methods 14, 607–614 (2017).
Lazzarotto, C. R. et al. CHANGE-seq reveals genetic and epigenetic effects on CRISPR–Cas9 genome-wide activity. Nat. Biotechnol. 38, 1317–1327 (2020). CHANGE-seq establishes a streamlined, high-throughput, biochemical method to define the genome-wide activity of CRISPR genome editors, by selective sequencing of editor-modified genomic DNA.
Petri, K. et al. Global-scale CRISPR gene editor specificity profiling by ONE-seq identifies population-specific, variant off-target effects. Preprint at bioRxiv https://doi.org/10.1101/2021.04.05.438458 (2021).
Lazzarotto, C. R. et al. Sensitive and unbiased genome-wide profiling of base-editor-induced off-target activity using CHANGE-seq-BE. Nat. Biotechnol. https://doi.org/10.1038/s41587-025-02948-7 (2026).
Ramadoss, G. N. et al. Characterizing and controlling CRISPR repair outcomes in nondividing human cells. Nat. Commun. 16, 9883 (2025). This study compares derived neurons to parental iPS cells and reveals differences in reparative responses to Cas9-induced DNA damage, raising opportunities to direct towards specific editing outcomes.
Yan, W. X. et al. BLISS is a versatile and quantitative method for genome-wide profiling of DNA double-strand breaks. Nat. Commun. 8, 15058 (2017).
Tsai, S. Q. et al. GUIDE-seq enables genome-wide profiling of off-target cleavage by CRISPR-Cas nucleases. Nat. Biotechnol. 33, 187–197 (2015).
Wienert, B., Wyman, S. K., Yeh, C. D., Conklin, B. R. & Corn, J. E. CRISPR off-target detection with DISCOVER-seq. Nat. Protoc. 15, 1775–1799 (2020).
Liang, S.-Q. et al. Genome-wide profiling of prime editor off-target sites in vitro and in vivo using PE-tag. Nat. Methods 20, 898–907 (2023).
Liang, S.-Q. et al. Genome-wide detection of CRISPR editing in vivo using GUIDE-tag. Nat. Commun. 13, 437 (2022).
Turchiano, G. et al. Quantitative evaluation of chromosomal rearrangements in gene-edited human stem cells by CAST-seq. Cell Stem Cell 28, 1136–1147.e5 (2021).
Kwon, J. et al. TAPE-seq is a cell-based method for predicting genome-wide off-target effects of prime editor. Nat. Commun. 13, 7975 (2022).
Cromer, M. K. et al. Comparative analysis of CRISPR off-target discovery tools following ex vivo editing of CD34+ hematopoietic stem and progenitor cells. Mol. Ther. 31, 1074–1087 (2023).
Doman, J. L., Raguram, A., Newby, G. A. & Liu, D. R. Evaluation and minimization of Cas9-independent off-target DNA editing by cytosine base editors. Nat. Biotechnol. 38, 620–628 (2020).
Zuo, E. et al. Cytosine base editor generates substantial off-target single-nucleotide variants in mouse embryos. Science 364, 289–292 (2019).
Grünewald, J. et al. Transcriptome-wide off-target RNA editing induced by CRISPR-guided DNA base editors. Nature 569, 433–437 (2019).
Cancellieri, S. et al. Human genetic diversity alters off-target outcomes of therapeutic gene editing. Nat. Genet. 55, 34–43 (2023).
Li, M. & Izpisua Belmonte, J. C. Organoids – preclinical models of human disease. N. Engl. J. Med. 380, 569–579 (2019).
US FDA. Roadmap to reducing animal testing in preclinical safety studies. https://www.fda.gov/media/186092/download (2025).
Takahashi, K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131, 861–872 (2007).
Schwank, G. et al. Functional repair of CFTR by CRISPR/Cas9 in intestinal stem cell organoids of cystic fibrosis patients. Cell Stem Cell 13, 653–658 (2013).
Matano, M. et al. Modeling colorectal cancer using CRISPR–Cas9-mediated engineering of human intestinal organoids. Nat. Med. 21, 256–262 (2015).
Geurts, M. H. et al. CRISPR-based adenine editors correct nonsense mutations in a cystic fibrosis organoid biobank. Cell Stem Cell 26, 503–510.e7 (2020). This state-of-the art study demonstrates how a cystic fibrosis intestinal organoid biobank can be applied to profile base editing on-target and off-target biological effects.
Schene, I. F. et al. Prime editing for functional repair in patient-derived disease models. Nat. Commun. 11, 5352 (2020).
Lee, H. & Kim, J.-S. Unexpected CRISPR on-target effects. Nat. Biotechnol. 36, 703–704 (2018).
Boutin, J. et al. ON-Target adverse events of CRISPR–Cas9 nuclease: more chaotic than expected. CRISPR J. 5, 19–30 (2022).
Friskes, A. et al. Double-strand break toxicity is chromatin context independent. Nucleic Acids Res 50, 9930–9947 (2022).
Baruteau, J., Waddington, S. N., Alexander, I. E. & Gissen, P. Gene therapy for monogenic liver diseases: clinical successes, current challenges and future prospects. J. Inherit. Metab. Dis. 40, 497–517 (2017).
Artegiani, B. et al. Fast and efficient generation of knock-in human organoids using homology-independent CRISPR–Cas9 precision genome editing. Nat. Cell Biol. 22, 321–331 (2020). The authors report the development of a homology-independent CRISPR method to efficiently generate knock-in organoids of both intestinal and hepatocyte lineages for mechanistic investigations.
Velazquez, J. J. et al. Gene regulatory network analysis and engineering directs development and vascularization of multilineage human liver organoids. Cell Syst. 12, 41–55.e11 (2021).
Zhang, Y. et al. A new 3D cultured liver chip and real-time monitoring system based on microfluidic technology. Micromachines 11, 1118 (2020).
Lim, A. Y. et al. Reproducibility and robustness of a liver microphysiological system PhysioMimix LC12 under varying culture conditions and cell type combinations. Bioeng. 10, 1195 (2023).
Fu, J., Qiu, H. & Tan, C. S. Microfluidic liver-on-a-chip for preclinical drug discovery. Pharmaceutics 15, 1300 (2023).
Pineda, M., Moghadam, F., Ebrahimkhani, M. R. & Kiani, S. Engineered CRISPR systems for next generation gene therapies. ACS Synth. Biol. 6, 1614–1626 (2017).
Hernandez-Gordillo, V., Casolaro, T. C., Ebrahimkhani, M. R. & Kiani, S. Multicellular systems to translate somatic cell genome editors to humans. Curr. Opin. Biomed. Eng. 16, 72–81 (2020).
Connaughton, D. M. et al. Monogenic causes of chronic kidney disease in adults. Kidney Int. 95, 914–928 (2019).
Freedman, B. S. et al. Modelling kidney disease with CRISPR-mutant kidney organoids derived from human pluripotent epiblast spheroids. Nat. Commun. 6, 8715 (2015).
Takasato, M. et al. Kidney organoids from human iPS cells contain multiple lineages and model human nephrogenesis. Nature 536, 238 (2016).
Taguchi, A. et al. Redefining the in vivo origin of metanephric nephron progenitors enables generation of complex kidney structures from pluripotent stem cells. Cell Stem Cell 14, 53–67 (2014).
Morizane, R. et al. Nephron organoids derived from human pluripotent stem cells model kidney development and injury. Nat. Biotechnol. 33, 1193–1200 (2015).
Czerniecki, S. M. et al. High-throughput screening enhances kidney organoid differentiation from human pluripotent stem cells and enables automated multidimensional phenotyping. Cell Stem Cell 22, 929–940.e4 (2018).
Li, S. R. et al. Glucose absorption drives cystogenesis in a human organoid-on-chip model of polycystic kidney disease. Nat. Commun. 13, 7918 (2022).
Hiratsuka, K. et al. Organoid-on-a-chip model of human ARPKD reveals mechanosensing pathomechanisms for drug discovery. Sci. Adv. 8, eabq0866 (2022).
Zhang, Z. et al. Detection of PKD1 and PKD2 somatic variants in autosomal dominant polycystic kidney cyst epithelial cells by whole-genome sequencing. J. Am. Soc. Nephrol. 32, 3114–3129 (2021).
Cruz, N. M. et al. Organoid cystogenesis reveals a critical role of microenvironment in human polycystic kidney disease. Nat. Mater. 16, 1112–1119 (2017).
Xu, Y. et al. Adult human kidney organoids originate from CD24+ cells and represent an advanced model for adult polycystic kidney disease. Nat. Genet. 54, 1690–1701 (2022).
Schutgens, F. et al. Tubuloids derived from human adult kidney and urine for personalized disease modeling. Nat. Biotechnol. 37, 303–313 (2019).
Zuk, A. & Bonventre, J. V. Acute kidney injury. Annu. Rev. Med. 67, 293–307 (2016).
Vanslambrouck, J. M. et al. Enhanced metanephric specification to functional proximal tubule enables toxicity screening and infectious disease modelling in kidney organoids. Nat. Commun. 13, 5943 (2022).
Digby, J. L. M., Vanichapol, T., Przepiorski, A., Davidson, A. J. & Sander, V. Evaluation of cisplatin-induced injury in human kidney organoids. Am. J. Physiol. Ren. Physiol. 318, F971–F978 (2020).
Gupta, N. et al. Modeling injury and repair in kidney organoids reveals that homologous recombination governs tubular intrinsic repair. Sci. Transl. Med. 14, eabj4772 (2022).
Taguchi, K. et al. Cyclin G1 induces maladaptive proximal tubule cell dedifferentiation and renal fibrosis through CDK5 activation. J. Clin. Invest. 132, e158096 (2022).
Liu, E. et al. Profiling APOL1 nephropathy risk variants in genome-edited kidney organoids with single-cell transcriptomics. Kidney 360, 203–215 (2020).
Juliar, B. A. et al. Interferon-γ induces combined pyroptotic angiopathy and APOL1 expression in human kidney disease. Cell Rep. 43, 114310 (2024).
Thomson, R. et al. Evolution of the primate trypanolytic factor APOL1. Proc. Natl Acad. Sci. USA 111, E2130–E2139 (2014).
Helms, L. et al. Cross-validation of SARS-CoV-2 responses in kidney organoids and clinical populations. JCI Insight 6, e154882 (2021).
Monteil, V. et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell 181, 905–913.e7 (2020).
Sharmin, S. et al. Human induced pluripotent stem cell-derived podocytes mature into vascularized glomeruli upon experimental transplantation. J. Am. Soc. Nephrol. 27, 1778–1791 (2016).
van den Berg, C. W. et al. Renal subcapsular transplantation of PSC-Derived kidney organoids induces neo-vasculogenesis and significant glomerular and tubular maturation in vivo. Stem Cell Rep. 10, 751–765 (2018).
Grambergs, R. C., Mondal, K. & Mandal, N. Inflammatory ocular diseases and sphingolipid signaling. Adv. Exp. Med. Biol. 1159, 139–152 (2019).
Hanany, M., Rivolta, C. & Sharon, D. Worldwide carrier frequency and genetic prevalence of autosomal recessive inherited retinal diseases. Proc. Natl Acad. Sci. USA 117, 2710–2716 (2020).
Russell, S. et al. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet 390, 849–860 (2017).
Bulte, J. W. M. & Daldrup-Link, H. E. Clinical tracking of cell transfer and cell transplantation: trials and tribulations. Radiology 289, 604–615 (2018).
Berg, E. et al. Total-body PET and highly stable chelators together enable meaningful 89Zr-antibody PET studies up to 30 days after injection. J. Nucl. Med. 61, 453–460 (2020).
Huang, J., Lee, C. C. I., Sutcliffe, J. L., Cherry, S. R. & Tarantal, A. F. Radiolabeling rhesus monkey CD34+ hematopoietic and mesenchymal stem cells with 64Cu-pyruvaldehyde-bis(N4-methylthiosemicarbazone) for microPET imaging. Mol. Imaging 7, 1–11 (2008).
Tarantal, A. F. et al. Radiolabeling and in vivo imaging of transplanted renal lineages differentiated from human embryonic stem cells in fetal rhesus monkeys. Mol. Imaging Biol. 14, 197–204 (2012).
Tarantal, A. F., Lee, C. C. I., Kukis, D. L. & Cherry, S. R. Radiolabeling human peripheral blood stem cells for positron emission tomography (PET) imaging in young rhesus monkeys. PLoS ONE 8, e77148 (2013).
Bulte, J. W. M. Direct versus indirect labeling for chimeric antigen receptor T-cell tracking using PET. Radiology 310, e240241 (2024).
Yuan, Y. et al. In vivo tracking of unlabelled mesenchymal stromal cells by mannose-weighted chemical exchange saturation transfer MRI. Nat. Biomed. Eng. 6, 658–666 (2022). This study introduces a technique for label-free tracking of transplanted stem cells in vivo.
Badawi, R. D. et al. First human imaging studies with the EXPLORER Total-Body PET scanner. J. Nucl. Med. 60, 299–303 (2019).
Cherry, S. R. et al. Total-body imaging: Transforming the role of positron emission tomography. Sci. Transl. Med. 9, eaaf6169 (2017).
Mason, E. E. et al. Concept for using magnetic particle imaging for intraoperative margin analysis in breast-conserving surgery. Sci. Rep. 11, 13456 (2021).
Liu, S., Su, Y., Lin, M. Z. & Ronald, J. A. Brightening up biology: advances in luciferase systems for in vivo imaging. ACS Chem. Biol. 16, 2707–2718 (2021).
He, S. et al. EWS-FLI1-mediated tenascin-C expression promotes tumour progression by targeting MALAT1 through integrin α5β1-mediated YAP activation in Ewing sarcoma. Br. J. Cancer 121, 922–933 (2019).
Xu, Y. et al. PNCK depletion inhibits proliferation and induces apoptosis of human nasopharyngeal carcinoma cells in vitro and in vivo. J. Cancer 10, 6925–6932 (2019).
Mou, H. et al. CRISPR-SONIC: targeted somatic oncogene knock-in enables rapid in vivo cancer modeling. Genome Med 11, 21 (2019).
Chen, S.-H. et al. ABL genomic editing sufficiently abolishes oncogenesis of human chronic myeloid leukemia cells in vitro and in vivo. Cancers 12, 1399 (2020).
Meca-Cortés, O. et al. CRISPR/Cas9-mediated knockin application in cell therapy: a non-viral procedure for bystander treatment of glioma in mice. Mol. Ther. Nucleic Acids 8, 395–403 (2017).
Dubois, V. P. et al. Safe harbor targeted CRISPR–Cas9 tools for molecular-genetic imaging of cells in living subjects. CRISPR J. 1, 440–449 (2018).
Kelly, J. J. et al. Safe harbor-targeted CRISPR–Cas9 homology-independent targeted integration for multimodality reporter gene-based cell tracking. Sci. Adv. 7, eabc3791 (2021). This study demonstrates a CRISPR approach for safe-harbour integration of large multimodal imaging reporter constructs, enabling a viral-free, non-invasive strategy for longitudinal tracking of genome-edited cells in vivo.
Fu, P.-F. et al. CRISPR/Cas9-based generation of a recombinant double-reporter pseudorabies virus and its characterization in vitro and in vivo. Vet. Res. 52, 95 (2021).
Uyar, O. et al. A novel bioluminescent herpes simplex virus 1 for in vivo monitoring of herpes simplex encephalitis. Sci. Rep. 11, 18688 (2021).
Lau, C.-H., Ho, J. W.-T., Lo, P. K. & Tin, C. Targeted transgene activation in the brain tissue by systemic delivery of engineered AAV1 expressing CRISPRa. Mol. Ther. Nucleic Acids 16, 637–649 (2019).
Yu, S.-Y. et al. A luciferase reporter mouse model to optimize in vivo gene editing validated by lipid nanoparticle delivery of adenine base editors. Mol. Ther. 31, 1159–1166 (2023).
Amoasii, L. et al. In vivo non-invasive monitoring of dystrophin correction in a new Duchenne muscular dystrophy reporter mouse. Nat. Commun. 10, 4537 (2019).
Guo, Y. et al. A bioluminescence reporter mouse strain for in vivo imaging of CD8+ T cell localization and function. Biochem. Biophys. Res. Commun. 581, 12–19 (2021).
Tarantal, A. F. & Lee, C. C. I. Long-term luciferase expression monitored by bioluminescence imaging after adeno-associated virus-mediated fetal gene delivery in rhesus monkeys (Macaca mulatta). Hum. Gene Ther. 21, 143–148 (2010). This study uses BLI to monitor long-term reporter gene expression in rhesus monkeys after prenatal intrathoracic administration.
Tarantal, A. F., Lee, C. C. I., Martinez, M. L., Asokan, A. & Samulski, R. J. Systemic and persistent muscle gene expression in rhesus monkeys with a liver de-targeted adeno-associated virus vector. Hum. Gene Ther. 28, 385–391 (2017). This study demonstrates liver detargeting with an AAV9 variant after intravenous administration to infant rhesus monkeys with BLI monitoring expression for ~2 years post transfer.
Oh, Y. et al. An orange calcium-modulated bioluminescent indicator for non-invasive activity imaging. Nat. Chem. Biol. 15, 433–436 (2019).
Tarantal, A. F., Lee, C. C. I., Jimenez, D. F. & Cherry, S. R. Fetal gene transfer using lentiviral vectors: in vivo detection of gene expression by microPET and optical imaging in fetal and infant monkeys. Hum. Gene Ther. 17, 1254–1261 (2006).
Tarantal, A. F. & Skarlatos, S. I. Center for Fetal Monkey Gene Transfer for Heart, Lung, and Blood Diseases: an NHLBI resource for the gene therapy community. Hum. Gene Ther. 23, 1130–1135 (2012).
Bulte, J. W. M. & Kraitchman, D. L. Iron oxide MR contrast agents for molecular and cellular imaging. NMR Biomed. 17, 484–499 (2004).
Chapelin, F. et al. Fluorine-19 nuclear magnetic resonance of chimeric antigen receptor T cell biodistribution in murine cancer model. Sci. Rep. 7, 17748 (2017).
Dubois, V. P., Sehl, O. C., Foster, P. J. & Ronald, J. A. Visualizing CAR-T cell immunotherapy using 3 Tesla fluorine-19 MRI. Mol. Imaging Biol. 24, 298–308 (2022).
Bulte, J. W. M. Chimeric antigen receptor T-cell immunotherapy induces transient tumor hyperoxia instead of hypoxia. Radio. Imaging Cancer 3, e200135 (2021).
Gilad, A. A. et al. Artificial reporter gene providing MRI contrast based on proton exchange. Nat. Biotechnol. 25, 217–219 (2007). This study presents a non-metallic man-made reporter gene that can be detected directly.
Meier, S. et al. Non-invasive detection of adeno-associated viral gene transfer using a genetically encoded CEST-MRI reporter gene in the murine heart. Sci. Rep. 8, 4638 (2018).
Lam, B. et al. Imaging of adeno-associated viral capsids for purposes of gene editing using CEST NMR/MRI. Magn. Reson. Med. 92, 792–806 (2024). This study harnesses the outwardly facing amino acids on AAV capsids as an endogenous source of CEST-MRI contrast to quantify the delivery of gene-editing machinery via AAV particles to solid tissue.
Perlman, O. et al. Quantitative imaging of apoptosis following oncolytic virotherapy by magnetic resonance fingerprinting aided by deep learning. Nat. Biomed. Eng. 6, 648–657 (2022).
Bulte, J. W. M., Wang, C. & Shakeri-Zadeh, A. In vivo cellular magnetic imaging: labeled vs. unlabeled cells. Adv. Funct. Mater. 32, 2207626 (2022).
Bulte, J. W. M. et al. Quantitative ‘hot spot’ imaging of transplanted stem cells using superparamagnetic tracers and magnetic particle imaging (MPI). Tomography 1, 91–97 (2015). This study presents quantitative MPI/MRI cell tracking.
Bulte, J. W. M. Superparamagnetic iron oxides as MPI tracers: a primer and review of early applications. Adv. Drug Deliv. Rev. 138, 293–301 (2019).
Shakeri-Zadeh, A. et al. Fast dynamic whole-body in vivo cytometry using magnetic particle imaging. Preprint at bioRxiv https://doi.org/10.1101/2025.09.11.675624 (2025).
Kiru, L. et al. In vivo imaging of nanoparticle-labeled CAR T cells. Proc. Natl Acad. Sci. USA 119, e2102363119 (2022).
Shakeri-Zadeh, A. et al. MPI of SuperSPIO20-labeled ALS patient-derived, genome-edited iPSCs and iPSC-derived motor neurons. Int. J. Mag. Part. Imag. 8, 2203003 (2022).
Rossano, S. et al. Imaging the fetal nonhuman primate brain with SV2A positron emission tomography (PET). Eur. J. Nucl. Med. Mol. Imaging 49, 3679–3691 (2022).
Sheng, G. et al. P2RX7 promotes osteosarcoma progression and glucose metabolism by enhancing c-Myc stabilization. J. Transl. Med. 21, 132 (2023).
Marciano, S. et al. Combining CRISPR–Cas9 and brain imaging to study the link from genes to molecules to networks. Proc. Natl Acad. Sci. Usa. 119, e2122552119 (2022).
Hwang, I. et al. A radioactive CRISPR interference system using 89Zr-labeled LbCas12a. J. Control. Release 365, 703–715 (2024).
Herhaus, P. et al. Targeted positron emission tomography imaging of CXCR4 expression in patients with acute myeloid leukemia. Haematologica 101, 932–940 (2016).
Ostrominski, J. W. et al. CRISPR/Cas9-mediated introduction of the sodium/iodide symporter gene enables noninvasive in vivo tracking of induced pluripotent stem cell-derived cardiomyocytes. Stem Cells Transl. Med 9, 1203–1217 (2020).
Gao, Y. et al. CRISPR/Cas9-edited triple-fusion reporter gene imaging of dynamics and function of transplanted human urinary-induced pluripotent stem cell-derived cardiomyocytes. Eur. J. Nucl. Med. Mol. Imaging 48, 708–720 (2021).
Shalaby, N. et al. A Human-derived Dual MRI/PET reporter gene system with high translational potential for cell tracking. Mol. Imaging Biol. 24, 341–351 (2022).
Kulhankova, K. et al. Shuttle peptide delivers base editor RNPs to rhesus monkey airway epithelial cells in vivo. Nat. Commun. 14, 8051 (2023). This study uses chest CT to identify regions of deposited base editing reagents.
Liang, S.-Q. et al. AAV5 delivery of CRISPR/Cas9 mediates genome editing in the lungs of young rhesus monkeys. Hum. Gene Ther. 35, 814–824 (2024).
Hustedt, N. & Durocher, D. The control of DNA repair by the cell cycle. Nat. Cell Biol. 19, 1–9 (2016).
Zeng, J. et al. Gene editing without ex vivo culture evades genotoxicity in human hematopoietic stem cells. Cell Stem Cell 32, 191–208.e11 (2025).
Tsuchida, C. A. et al. Mitigation of chromosome loss in clinical CRISPR–Cas9-engineered T cells. Cell 186, 4567–4582.e20 (2023).
Freedman, B. S. Physiology assays in human kidney organoids. Am. J. Physiol. Ren. Physiol. 322, F625–F638 (2022).
Pamies, D. et al. Recommendations on fit-for-purpose criteria to establish quality management for microphysiological systems and for monitoring their reproducibility. Stem Cell Rep. 19, 1041 (2024).
Chu, V. T. et al. Increasing the efficiency of homology-directed repair for CRISPR–Cas9-induced precise gene editing in mammalian cells. Nat. Biotechnol. 33, 543–548 (2015).
Chen, Z. et al. A fluorescent reporter mouse for in vivo assessment of genome editing with diverse cas nucleases and prime editors. CRISPR J. 6, 570–582 (2023).
Maynard, L. H. et al. Fast-seq: a simple method for rapid and inexpensive validation of packaged single-stranded adeno-associated viral genomes in academic settings. Hum. Gene Ther. Methods 30, 195–205 (2019).
Homan, K. A. et al. Flow-enhanced vascularization and maturation of kidney organoids in vitro. Nat. Methods 16, 255–262 (2019).
Rizki-Safitri, A. et al. Live functional assays reveal longitudinal maturation of transepithelial transport in kidney organoids. Front. Cell Dev. Biol. 10, 978888 (2022).
Hunt, A. C. et al. Multivalent designed proteins neutralize SARS-CoV-2 variants of concern and confer protection against infection in mice. Sci. Transl. Med. 14, eabn1252 (2022).
Steyer, B. et al. Scarless genome editing of human pluripotent stem cells via transient puromycin selection. Stem Cell Rep. 10, 642–654 (2018).
Saha, K. Accounting for diversity in the design of CRISPR-based therapeutic genome editing. Nat. Genet. 55, 6–7 (2023).
Samimi, K. et al. In situ autofluorescence lifetime assay of a photoreceptor stimulus response in mouse retina and human retinal organoids. Biomed. Opt. Express 13, 3476–3492 (2022).
Wang, J. et al. Three-dimensional tissue-engineered human skeletal muscle model of Pompe disease. Commun. Biol. 4, 524 (2021).
Kwon, J. B. et al. In vivo gene editing of muscle stem cells with adeno-associated viral vectors in a mouse model of Duchenne muscular dystrophy. Mol. Ther. Methods Clin. Dev. 19, 320–329 (2020).
DeLuca, S. & Bursac, N. CRISPR library screening in cultured cardiomyocytes. Methods Mol. Biol. 2485, 1–13 (2022).
Chen, Z., Li, B., Zhan, R.-Z., Rao, L. & Bursac, N. Exercise mimetics and JAK inhibition attenuate IFN-γ-induced wasting in engineered human skeletal muscle. Sci. Adv. 7, eabd9502 (2021).
Helfer, A. & Bursac, N. Frame-hydrogel methodology for engineering highly functional cardiac tissue constructs. Methods Mol. Biol. 2158, 171–186 (2021).
Mao, M. et al. Redirecting vesicular transport to improve nonviral delivery of molecular cargo. Adv. Biosyst. 4, e2000059 (2020).
Kwon, J. B., Vankara, A., Ettyreddy, A. R., Bohning, J. D. & Gersbach, C. A. Myogenic progenitor cell lineage specification by CRISPR/Cas9-based transcriptional activators. Stem Cell Rep. 14, 755–769 (2020).
Samelson, A. J. et al. BRD2 inhibition blocks SARS-CoV-2 infection by reducing transcription of the host cell receptor ACE2. Nat. Cell Biol. 24, 24–34 (2022).
Fenix, A. M. et al. Gain-of-function cardiomyopathic mutations in RBM20 rewire splicing regulation and re-distribute ribonucleoprotein granules within processing bodies. Nat. Commun. 12, 6324 (2021).
Perez-Bermejo, J. A. et al. SARS-CoV-2 infection of human iPSC-derived cardiac cells reflects cytopathic features in hearts of patients with COVID-19. Sci. Transl. Med. 13, eabf7872 (2021).
Qian, T. et al. Label-free imaging for quality control of cardiomyocyte differentiation. Nat. Commun. 12, 4580 (2021).
Cheng, Y. & Tsai, S. Q. Illuminating the genome-wide activity of genome editors for safe and effective therapeutics. Genome Biol. 19, 226 (2018).
Métais, J.-Y. et al. Genome editing of HBG1 and HBG2 to induce fetal hemoglobin. Blood Adv. 3, 3379–3392 (2019).
Song, M. et al. Mapping cis-regulatory chromatin contacts in neural cells links neuropsychiatric disorder risk variants to target genes. Nat. Genet. 51, 1252–1262 (2019).
de Jong, J. O. et al. Cortical overgrowth in a preclinical forebrain organoid model of CNTNAP2-associated autism spectrum disorder. Nat. Commun. 12, 4087 (2021).
Bulcaen, M. et al. Prime editing functionally corrects cystic fibrosis-causing CFTR mutations in human organoids and airway epithelial cells. Cell Rep. Med. 5, 101544 (2024).
Liu, S. et al. Molecular imaging reveals a high degree of cross-seeding of spontaneous metastases in a novel mouse model of synchronous bilateral breast cancer. Mol. Imaging Biol. 24, 104–114 (2022).
Srivastava, A. K. et al. Serial in vivo imaging of transplanted allogeneic neural stem cell survival in a mouse model of amyotrophic lateral sclerosis. Exp. Neurol. 289, 96–102 (2017).
Shalaby, N. et al. Complementary early-phase magnetic particle imaging and late-phase positron emission tomography reporter imaging of mesenchymal stem cells in vivo. Nanoscale 15, 3408–3418 (2023).
Williams, R. J. et al. Dual magnetic particle imaging and akaluc bioluminescence imaging for tracking cancer cell metastasis. Tomography 9, 178–194 (2023).
Kim, T. et al. In Vivo Micro-CT imaging of human mesenchymal stem cells labeled with Gold-Poly-L-Lysine Nanocomplexes. Adv. Funct. Mater. 27, 1604213 (2017).
Farhadi, A., Ho, G. H., Sawyer, D. P., Bourdeau, R. W. & Shapiro, M. G. Ultrasound imaging of gene expression in mammalian cells. Science 365, 1469–1475 (2019).
Nyström, N. N., Yip, L. C. M., Carson, J. J. L., Scholl, T. J. & Ronald, J. A. Development of a human photoacoustic imaging reporter gene using the clinical dye indocyanine green. Radio. Imaging Cancer 1, e190035 (2019).
Emami-Shahri, N. et al. Clinically compliant spatial and temporal imaging of chimeric antigen receptor T-cells. Nat. Commun. 9, 1081 (2018).
Shalaby, N. et al. Imaging CAR-NK cells targeted to HER2 ovarian cancer with human sodium-iodide symporter-based positron emission tomography. Eur. J. Nucl. Med. Mol. Imaging 51, 3176–3190 (2024).
Nyström, N. N. et al. A genetically encoded magnetic resonance imaging reporter enables sensitive detection and tracking of spontaneous metastases in deep tissues. Cancer Res 83, 673–685 (2023).