Infants born with alternating hemiplegia of childhood (AHC) begin experiencing episodes of paralysis and seizures by the time they are a few months old, followed by developmental delays and intellectual disability. There is no cure or effective treatment for this rare genetic disease.
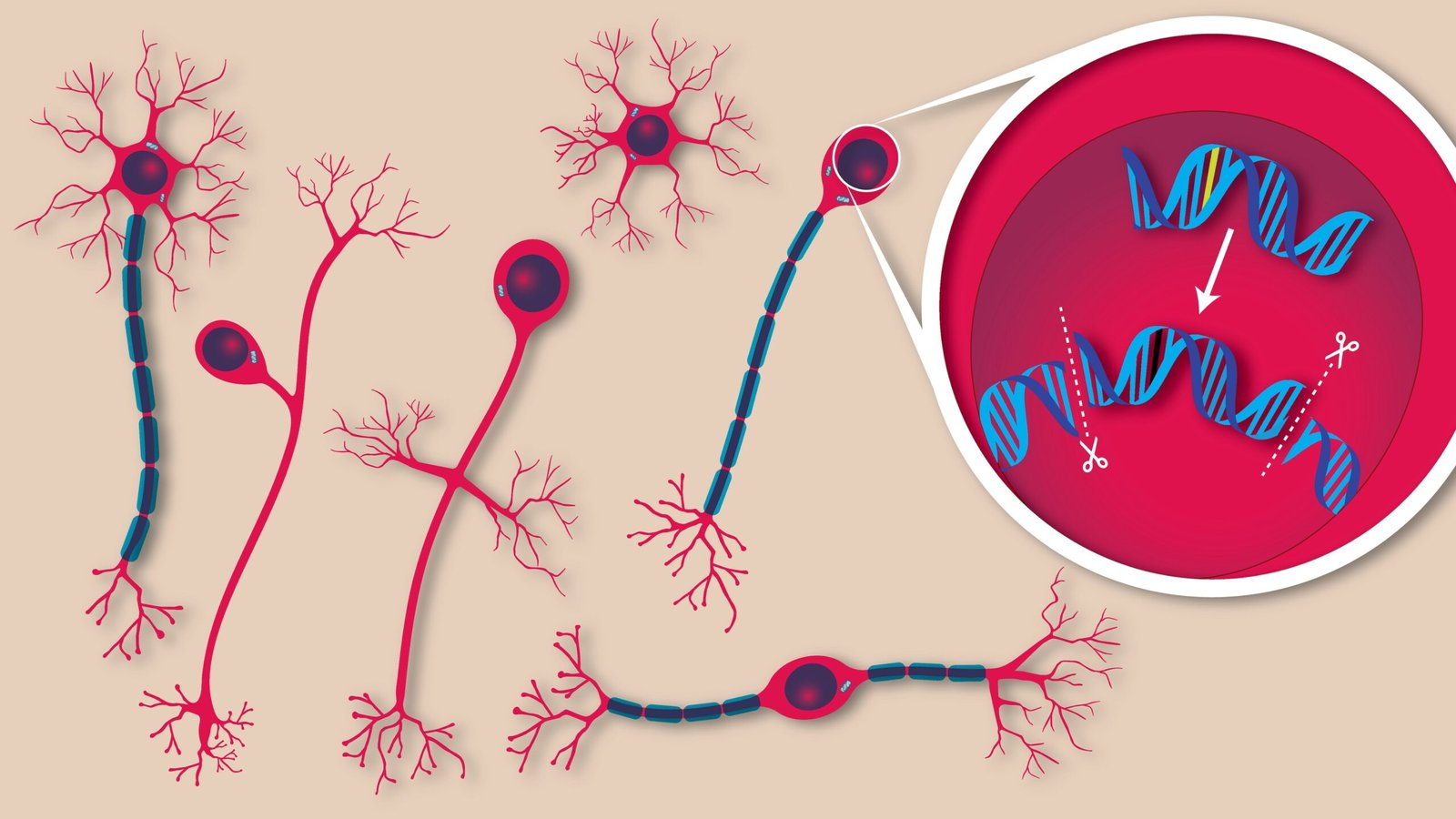
Now, researchers at the Broad Institute and the Jackson Laboratory have used prime editing to correct five different AHC-causing genetic mutations. Mice that received the treatment had fewer and less severe symptoms of AHC and survived more than twice as long as untreated mice. This work represents the first time prime editing has been used to treat a neurological disease in animals.
The new study is published in Cell, in the paper, “In vivo prime editing rescues alternating hemiplegia of childhood in mice.”
“This study is an important milestone for prime editing and one of the most exciting examples of therapeutic gene editing to come from our team,” said David Liu, PhD, a Broad core institute member, HHMI investigator, and professor at Harvard University. “It opens the door to one day repairing the underlying genetic causes of many neurological disorders that have long been considered untreatable.”
The vast majority of AHC cases are caused by one of four mutations in ATP1A3, a gene essential for brain cell function. The team set out to simultaneously develop prime editing treatments to correct five ATP1A3 mutations, including the four most common, a scale rarely attempted in therapeutic gene editing research.
“We developed a robust framework to correct multiple mutations in parallel,” said Alexander Sousa, PhD, a postdoctoral fellow in the Liu lab. “This effort was really about creating a blueprint that could be rapidly applied to other rare diseases, too.”
The researchers first tested their strategies in cultured cells from patients with AHC. They demonstrated that they could correctly repair AHC mutations in up to 90% of treated cells, with minimal changes to other stretches of DNA.
Next, the group collaborated with Jackson Lab researchers to test their AAV-delivered treatments in two mouse models of AHC, which carry Atp1a3 mutations. Without treatment, the mice developed seizures, movement problems, and died prematurely. When the scientists injected their editing system into the brains of the animals, their symptoms disappeared or were substantially reduced. Treated mice survived more than twice as long as untreated animals. Moreover, the function of their Atp1a3 protein was restored in the brain, and their motor and cognitive deficits were ameliorated.
The team also tested traditional gene therapy, which delivered a copy of the ATP1A3 gene to cells. In this experiment, symptoms did not improve in animals, highlighting the unique advantage of using gene editing to directly correct a mutation.
Because the treatment required direct injection into the brain shortly after birth, the team is now exploring less invasive delivery methods, and whether treatment later in life could still be effective.
“This is a powerful proof of concept,” said Holt Sakai, PhD, a postdoc in the Liu lab. “It shows that we can use prime editing to treat genetic brain diseases, and it lays the groundwork for translating this approach to the clinic.” The team sees their approach as a template for tackling other rare genetic diseases, especially those that affect the brain.
The team’s patient partner for this work is RARE Hope (formerly Hope for Annabel), a nonprofit focused on accelerating research on AHC and developing scalable, patient-centric research platforms to benefit the larger rare disease community. RARE Hope initiated the collaboration and was closely engaged throughout the project.
“This study is a win not just for our community but for all rare neurological conditions, and a breakthrough moment in expanding access to a broader cohort of potential patients,” said Nina Frost, founder and president of RARE Hope, a co-author of the study, and mother of a daughter with AHC. “It’s been a privilege to collaborate on such a scientifically significant effort with a team that has kept patients at the center of proof-of-concept research—engaging the patient community, modeling the patient experience, and integrating patient priorities into experimental design. This is a model for patient-relevant, patient-centered research because the team included us as true partners.”
The post Prime Editing Reverses Childhood Brain Disorder in Mouse Model appeared first on GEN – Genetic Engineering and Biotechnology News.